The healthcare business is changing quickly in 2025, and medical billing needs to keep up. Changes in regulations, complicated payer requirements, and the rise of value-based care are all changing the way revenue cycle management works.
Outdated billing practices often lead to delays, denials, and financial instability. To function well in this changing environment, healthcare providers need to use modern, integrated billing methods that improve accuracy, efficiency, and long-term viability.
In this blog, we will discuss 10 proven strategies to optimize medical billing in 2025, helping your practice stay competitive, compliant, and financially strong.
1. Enhance the Efficiency of Claim Submissions
Accurate and timely claim submission is vital for reducing denials and speeding reimbursements. Errors like incomplete information or incorrect coding often disrupt the payment process.
To improve efficiency, implement intelligent billing software that automates claim creation, identifies issues before submission, and tracks progress across payers. Standardized coding protocols and comprehensive documentation further ensure claims are clean and compliant.
Key strategies for smoother claim handling:
- Provide ongoing training for billing staff
- Use batch processing to manage high claim volumes
- Add a final review step to catch errors early
Not only does the simplified claims process cut down on documentation, but it also increases cash flow and overall revenue performance.
2. Optimize Revenue Cycle with Smart Billing Technology
Using AI-powered billing software changes medical billing by automating routine chores, cutting down on mistakes made by hand, and making the whole process more efficient.
These intelligent systems detect coding issues in real time, flag missing documentation, and predict claim outcomes based on historical trends, resulting in faster reimbursements and fewer denials.
Additionally, integrated analytics and customizable reporting tools offer valuable insights for better financial decision-making. Embracing advanced billing technology not only lightens administrative burdens but also lays the groundwork for sustainable revenue growth.
3. Empower Your Team Through Continuous Training
In today’s fast-changing healthcare environment, continuous staff education is crucial for maintaining accurate and efficient billing processes. With evolving coding standards and payer requirements, well-informed billing teams are essential to prevent errors and ensure compliance.
Regular training via workshops, webinars, and certification programs keeps staff up to date on ICD-10/11 updates, CPT code changes, and payer-specific rules. A knowledgeable team improves claim accuracy, reduces denials, and accelerates reimbursement. Fostering a culture of learning also boosts morale, confidence, and overall performance.
4. Stay Ahead with Proactive Regulatory Compliance
Keeping up with regulatory changes is fundamental to effective medical billing. As the industry shifts toward ICD-11 and undergoes frequent CPT and payer policy updates, staying informed is key to avoiding compliance risks and revenue disruptions.
Implementing proactive measures such as subscribing to CMS updates, engaging with industry associations, and appointing a compliance officer. This helps practices adapt billing procedures in real time. Staying ahead of regulatory changes safeguards your practice against penalties and supports long-term financial health.
5. Strengthen Financial Transparency with Patients
Proactive, transparent communication about billing policies, insurance coverage, and payment expectations helps prevent confusion and delays. Providing clear, easy-to-read billing statements and flexible payment plans builds patient trust and improves collection rates.
Discussing costs early in the care process also reduces the likelihood of disputes and fosters a more positive financial experience.
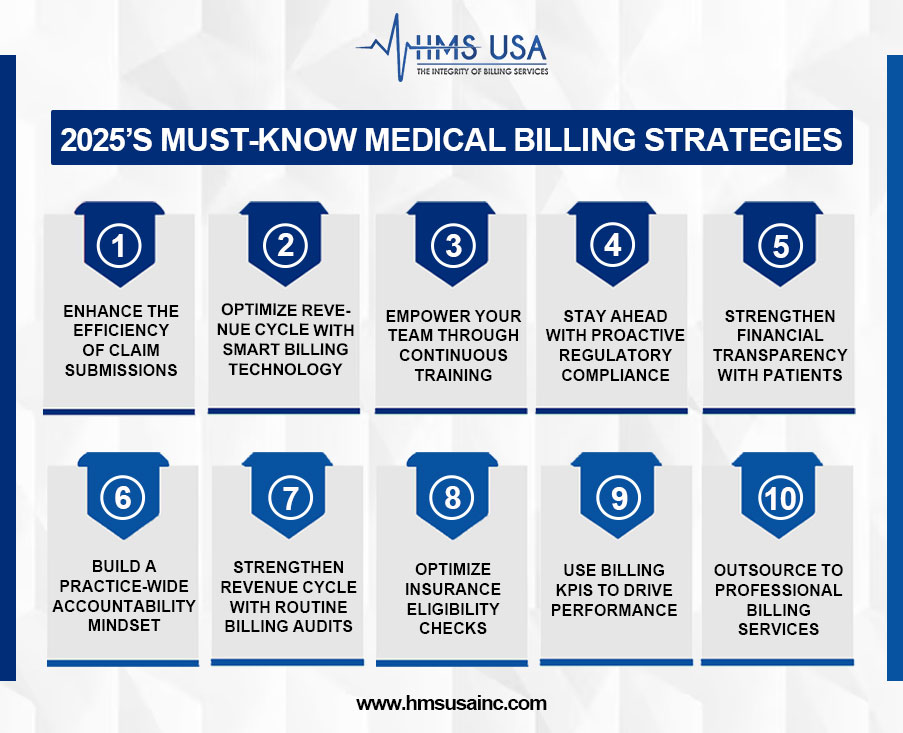
6. Build a Practice-Wide Accountability Mindset
A coordinated team effort is necessary for successful medical billing. Including all staff members, who include clinical, administrative, and billing, in revenue cycle duties helps ensure consistency and accuracy.
Establish performance benchmarks, track key metrics, and conduct regular reviews to drive continuous improvement.
A culture of accountability ensures the timely identification of issues and supports long-term financial performance.
7. Strengthen Revenue Cycle with Routine Billing Audits
Consistent internal audits are essential for identifying billing errors, compliance gaps, and process inefficiencies. They also reveal recurring issues that may signal deeper revenue cycle problems.
Whether performed monthly, quarterly, or annually, audits help validate coding accuracy, ensure proper documentation, and assess billing workflow effectiveness. Use standardized audit checklists, involve cross-functional teams, and implement corrective actions to address findings.
This proactive strategy supports billing integrity, improves reimbursement rates, and reduces the risk of external audits.
8. Optimize Insurance Eligibility Checks
Timely and accurate insurance verification is key to preventing claim denials and ensuring smooth billing operations. Confirming coverage, co-pays, and prior authorizations before appointments minimizes payment delays and improves patient satisfaction.
Integrate real-time eligibility tools with your practice management system to automate checks and reduce manual errors.
Train front-desk staff to verify insurance details during scheduling and check-in. Consistent eligibility verification ensures clean claims and accelerates cash flow.
9. Use Billing KPIs to Drive Performance
Tracking Key Performance Indicators (KPIs) provides actionable insights for improving medical billing operations. Focus on:
- Denial Rate – High rates often point to coding or eligibility issues.
- Days in A/R – Long collection cycles may indicate workflow inefficiencies.
- Clean Claim Rate – A high rate shows claims are submitted correctly the first time.
Regularly monitor these metrics using dashboards and reporting tools. Analyzing trends enables better decision-making, faster reimbursements, and sustained revenue growth.
10. Outsource to Professional Billing Services (If Needed)
Outsourcing medical billing can be a smart move, especially for clinics that have trouble with inefficiency, high denial rates, or not having enough staff. If your internal teams are too busy, it’s hard to keep up with compliance rules, or your cash flow is erratic, it could be time to think about outsourcing.
By working with specialised billing businesses, you may get help from experienced personnel, cutting-edge technology, and full knowledge of revenue cycle management.
These providers keep up with the newest changes in rules, payer regulations, and coding standards to cut down on mistakes and get the most money back.
Outsourcing lets clinics focus more on taking care of patients while making sure that their finances are all in order and legal.
Conclusion
Medical billing can be considerably improved by using proper strategies, including outsourcing, better contact with patients, and encouraging accountability. These techniques help lower mistakes, speed up payments, and make patients happier.
Because the healthcare market is always changing, practices need to customize these methods to stay competitive in 2025 and beyond.
If your practice is looking to enhance billing performance and streamline revenue cycle operations, consider seeking expert support.
For tailored solutions and professional guidance, contact HMS Group Inc.—a trusted name in medical billing optimization. Explore more medical billing tips and tricks, and let HMS Group Inc. help you achieve accuracy, efficiency, and compliance in every claim.








