Medical credentialing plays a vital role in ensuring healthcare providers are qualified and prepared to deliver safe, high-quality care. Studies show that nearly 30% of medical claims are delayed or denied due to credentialing errors, resulting in significant costs for providers in terms of time and revenue.
The credentialing process is more complex than ever, as healthcare continues to evolve rapidly due to the introduction of new tools and stricter regulations. That’s why the 2025 update aims to simplify credentialing, reduce paperwork, and improve accuracy, helping to restore patient trust and streamline healthcare delivery.
A better, more dependable healthcare system for everybody depends on this update, which is a necessary initial step. Let’s dive a bit deeper in this update.
What is Credentialing?
Credentialing in healthcare is a systematic process that verifies a provider’s qualifications, including education, training, licenses, certifications, and professional history. It also involves background checks for malpractice and disciplinary actions.
This process is essential not only for compliance but also as a critical safeguard to ensure that providers are competent and legally authorized to deliver care. Proper credentialing protects patient safety, promotes high-quality care, reduces risks and liability, and builds trust among patients, insurers, and regulators. It serves as a key defense in maintaining clinical excellence within healthcare organizations.
Key Medical Credentialing Changes in 2025
The year 2025 has introduced significant changes in medical credentialing, driven by technological advancements, regulatory updates, and a push for digital integration. These developments focus on streamlining workflows, improving transparency, and ensuring compliance with modern healthcare standards.
Technology Advancements and Compliance
Advanced credentialing software, powered by AI and machine learning, now automates tasks such as primary source verification, license monitoring, and ongoing compliance checks. This reduces administrative workload and errors. Meanwhile, new federal mandates, including updates from CMS, enforce stricter verification of malpractice and disciplinary histories to enhance patient safety.
Evolving Verification Processes
Verification has shifted toward real-time data synchronization. Health systems perform more frequent audits and background checks using integrated digital tools, enabling quicker access to accurate provider information and faster credentialing decisions.
Integration with National Databases
Credentialing platforms are now required to integrate with national databases, such as the National Practitioner Data Bank (NPDB) and the Federation of State Medical Boards (FSMB). This centralizes provider information, speeds up verification, and mandates providers keep their profiles current to maintain good standing.
Impact on Providers and Facilities
Credentialing changes have significantly impacted healthcare providers and facilities, transforming administrative workflows and raising new compliance, documentation, and electronic record-keeping requirements.
- Credentialing shifted from paper to digital platforms.
- Providers must stay digitally prepared.
- Shorter initial and recredentialing timelines.
- More detailed documentation is required.
- Private practices face higher admin costs.
- Digital systems improve long-term efficiency.
- Hospitals invest in integrated credentialing solutions.
- Remote providers face complex cross-state verification.
- Telemedicine compacts ease multi-state credentialing.
2025 Medicaid Credentialing Updates: What Providers Need to Know
As of 2025, Medicaid credentialing has undergone significant changes affecting new enrollments and revalidations. These updates reflect CMS’s focus on streamlining enrollment, strengthening program integrity, and improving patient access.
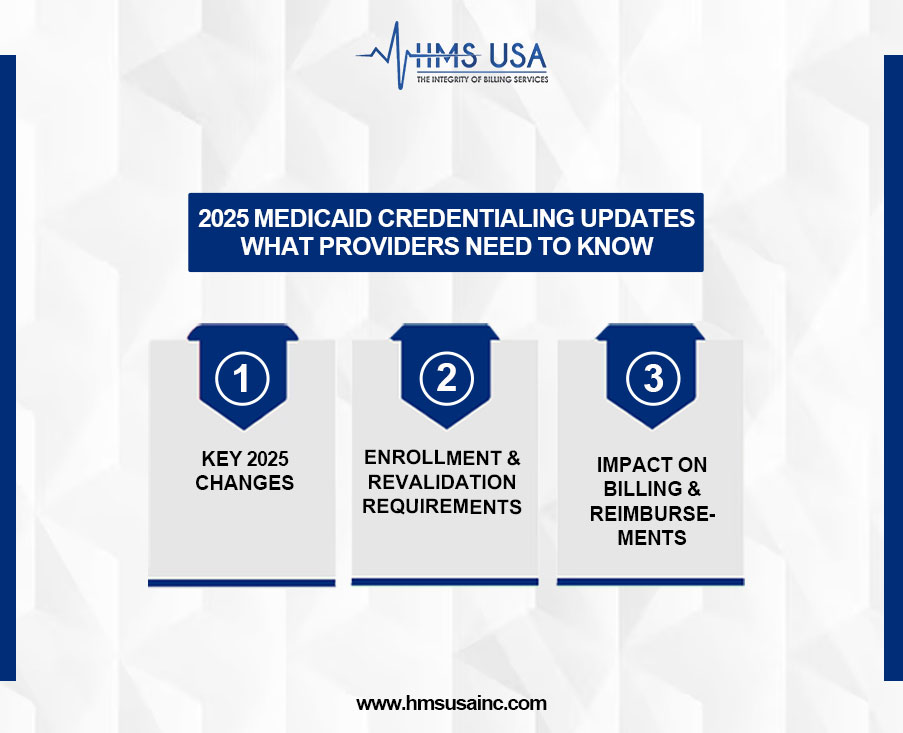
Key 2025 Changes
- Introduction of digital verification tools and stricter background checks.
- Tighter submission deadlines and mandatory compliance training.
- States must follow updated federal guidelines emphasizing transparency and accurate provider data.
Enrollment & Revalidation Requirements
- Providers must submit complete applications, including licensure, malpractice insurance, and NPI confirmation.
- PECOS is now required for electronic submissions in most states, reducing errors.
- Revalidation must begin at least 90 days before expiration; delays can result in suspension.
- Ongoing credential monitoring is now standard.
Impact on Billing & Reimbursements
- Delays or incomplete credentialing may lead to claim denials or payment holds.
- Real-time credential verification is now linked to billing.
- Improved compliance reduces audit risks and supports smoother payment processes.
- Coordination between the billing and credentialing teams is crucial for maintaining a stable cash flow.
Credentialing and US Healthcare Reforms
Credentialing has evolved from a routine task into a critical element of healthcare policy, driven by reforms aimed at increasing accountability, improving outcomes, and ensuring equitable access to care.

Standardized Credentialing and Healthcare Reform
Healthcare initiatives, such as the Affordable Care Act (ACA), emphasize standardized credentialing to enhance provider transparency and support the delivery of value-based care. Tools like CAQH ProView streamline verification, reduce administrative burden, and improve care coordination—key goals of healthcare reform.
Policy Changes Influencing Provider Qualifications
New policies are redefining credentialing by requiring continuing education in areas such as health equity, telemedicine, and behavioral health. These standards ensure that providers are equipped to meet the demands of modern care.
Credentialing as a Gatekeeper for Network Participation
Stricter network adequacy rules now require insurers to include diverse, fully credentialed providers. Provider Credentialing plays a gatekeeping role, ensuring only qualified professionals can join public and private insurance networks.
Medical Insurance Credentialing and Enrollment Enhancements
The medical insurance credentialing and enrollment process is evolving rapidly in 2025, driven by the need for greater efficiency, accuracy, and provider satisfaction. Streamlined processes are reducing administrative burdens and enhancing workflow efficiency.
Healthcare organizations are experiencing faster credentialing turnaround times due to stronger collaboration with insurers, who now prioritize quick verifications and real-time updates, thereby minimizing care delays.
Credentialing software and automation tools have become essential. These platforms handle everything from application submission to compliance monitoring, reducing errors, ensuring
timely renewals, and offering valuable analytics. In 2025, adopting these technologies is critical for staying competitive and compliant.
Closing Thoughts
Healthcare workers must stay up-to-date with changes in medical doctors credentials and enrollment to ensure they are following the rules and providing uninterrupted care. The changes for 2025 indicate that the healthcare system is moving toward modernization and collaboration.
Providers can maintain a smooth operation and enhance their role as trusted partners in patient care by continually adapting to new regulations and technologies.
Modern credentialing systems aim to enhance patient outcomes, streamline operations, and minimize administrative delays, thereby representing a significant investment in the future of healthcare.
For expert guidance and support with the latest in medical insurance credentialing and enrollment, contact HMS Group Inc. Their team of credentialing professionals is equipped to help healthcare providers navigate regulatory updates and implement simple, automated solutions for long-term success.