Modifier 22 is one of the most misunderstood CPT modifiers in medical billing. It is used when a procedure requires significantly more work than usual, and providers deserve higher reimbursement for that increased complexity. However, incorrect usage of Modifier 22 leads to claim denials, payment delays, and compliance risks, which is why understanding proper guidelines is essential.
This complete guide explains the Modifier 22 description, when to use it, documentation requirements, payer expectations, and real Modifier 22 examples, giving healthcare practices a clear roadmap for compliant and successful billing.
What Is Modifier 22?
Modifier 22 Description
Modifier 22: also known as CPT Modifier 22 (Increased Procedural Services), is appended to a CPT code when a provider performs a procedure that is:
- More difficult
- More time-consuming
- More complex
- Requires significantly increased effort
In short, Modifier 22 informs payers that the procedure exceeded normal expectations, and additional reimbursement is justified.
What Does Modifier 22 Communicate?
“This procedure was unusually complex and required increased procedural services.”
When Modifier 22 Applies
Modifier 22 is appropriate when:
- The patient’s anatomy is unusually complex
- Unexpected complications occur
- The surgery requires additional dissection, repair, or time
- The procedure extends far beyond the typical duration
- Significant clinical challenges arise
Modifier 22 Examples
Example 1: Complex Appendectomy
A standard appendectomy becomes difficult due to extensive adhesions, leading to an extra 45 minutes of surgical time. This situation qualifies for Modifier 22.
Example 2: Hernia Repair With Unexpected Anatomy
A surgeon encounters unusual anatomical variations during a hernia repair that require additional dissection and heightened precision. Modifier 22 is warranted.
Example 3: Cholecystectomy With Excessive Bleeding
During a routine gallbladder removal, uncontrolled bleeding increases complexity and duration. This is a clear Modifier 22 scenario.
These Modifier 22 examples demonstrate procedures that exceed standard expectations and justify higher reimbursement.
When Should Modifier 22 Be Used?
Modifier 22 should only be used when extraordinary factors make the procedure significantly more challenging. Minor complications or slightly increased time do not qualify.
Appropriate Situations Include:
- Unusual patient anatomy
- Severe adhesions requiring extensive dissection
- Complications requiring additional operative steps
- Excessive bleeding
- Prolonged surgical duration
- Technical difficulty beyond CPT code expectations
Essential Documentation Requirements
Insurance carriers require clear, detailed proof that the procedure demanded more work.
Documentation must include:
- What made the procedure unusually complex
- How the case differed from the standard procedure
- Exact extra time spent
- Extra steps taken
- Any complicating patient factors
- Operative notes reflecting increased intensity
Without this documentation, Modifier 22 claims are denied 90% of the time.
Common Reasons for Using the 22 Modifier
Modifier 22 is justified when:
- The intensity of the procedure increases significantly
- The duration exceeds normal expectations
- The provider performs extra procedural components
- Unexpected pathology or anatomy makes the surgery difficult
- A complex clinical condition impacts the surgical approach
Selective, compliant use improves acceptance rates and avoids red flags.
Common Mistakes to Avoid With Modifier 22
Incorrect use of Modifier 22 leads to denials and compliance audits. The most frequent mistakes include:
Using Modifier 22 for minor variations
Small differences in time or technique do not qualify.
Poor documentation
If the note doesn’t justify higher intensity, payers automatically deny the claim.
Applying Modifier 22 to the wrong CPT code
It should only be appended to the primary CPT code.
Ignoring payer-specific rules
Some payers require additional time logs, comparisons, or operative notes.
Tips for Correct Use of Modifier 22
To ensure successful reimbursement, follow these best practices:
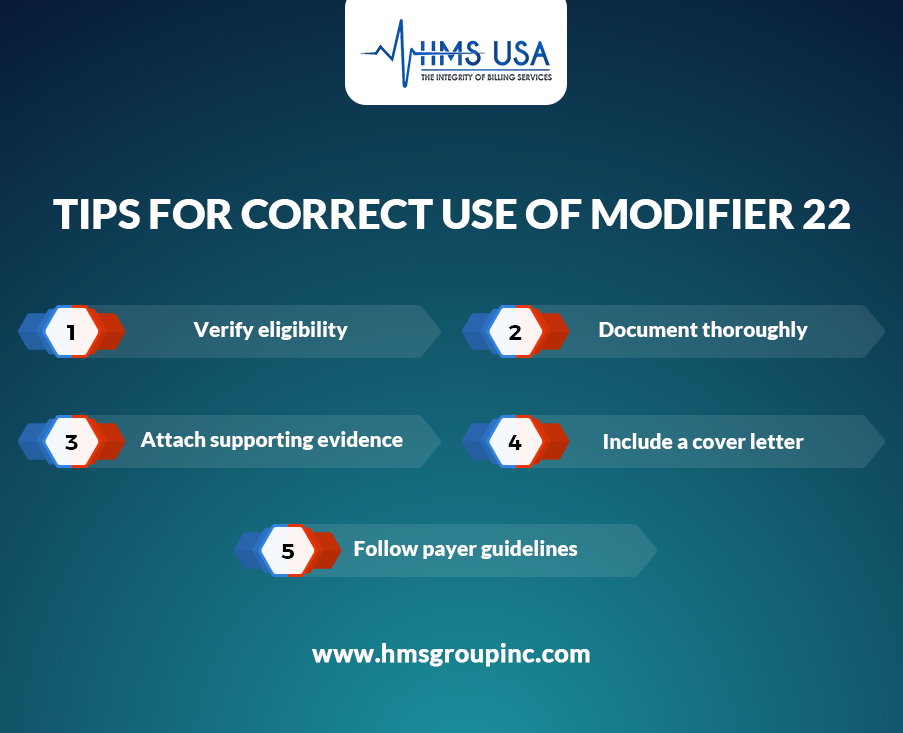
Verify eligibility
Confirm that the procedure required significantly more work.
Document thoroughly
Include clear, specific details, not generic statements.
Attach supporting evidence
Photos, imaging, pathology findings, or time logs strengthen the claim.
Include a cover letter
A concise justification letter increases approval odds.
Follow payer guidelines
Medicare, Medicaid, and private payers have different requirements.
Modifier 22 Guidelines
The official Modifier 22 guidelines emphasize compliance and accuracy:
- Append Modifier 22 only when complexity exceeds CPT expectations
- Use it only for the primary surgical procedure
- Ensure documentation supports increased procedural services
- Provide clinical relevance for complications
- Submit accompanying documentation upfront for faster adjudication
Correct use ensures fair reimbursement and reduces claim rework.
Payer-Specific Rules for Modifier 22
Each payer may apply different criteria:
- Medicare: Requires detailed operative notes and clear justification
- Commercial plans: May require pre-authorization or additional documentation
- Medicaid: Often enforces stricter review before approving additional payment
Regular payer updates ensure your Modifier 22 claims stay compliant and profitable.
Conclusion
Modifier 22 is a powerful tool for capturing fair reimbursement when a procedure requires increased procedural services. By understanding the Modifier 22 description, documentation requirements, payer rules, and proper usage, practices can avoid denials and ensure accurate payments. Correct use protects revenue, compliance, and clinical integrity.
For expert support with complex modifiers, clean claims, and compliant billing, HMS USA Inc. is your trusted partner for maximizing reimbursement.
FAQs
What is Modifier 22?
Modifier 22 is a CPT modifier used when a procedure requires significantly more time, effort, or complexity than usual.
When should Modifier 22 be used?
Use Modifier 22 only when unexpected complications, unusual anatomy, or increased surgical intensity make the procedure unusually difficult.
What documentation is required for Modifier 22?
Operative notes must detail what made the procedure harder, extra time spent, additional steps, and clinical justification.
Does Modifier 22 guarantee higher reimbursement?
No. Payers only increase payment if documentation clearly supports increased procedural services.
What are the common mistakes with Modifier 22?
Using it for minor issues, insufficient documentation, ignoring payer rules, or attaching it to the wrong code.








