The healthcare world in 2025 is moving fast, driven by new tech, changing regulations, and the push for value-based care. For specialty practices such as cardiology, orthopedics, or oncology, keeping up with accurate medical coding is now more challenging than ever.
That’s why more providers are turning to medical coding outsourcing. It’s a smart, scalable way to ensure compliance, boost efficiency, and tap into certified experts who know your specialty inside and out.
This blog will discuss how medical coding outsourcing helps specialty offices stay compliant, increase efficiency, and minimise administrative hassles. We’ll discuss how outsourcing provides professional solutions in today’s hectic healthcare industry.
What Is Medical Coding Outsourcing?
Medical coding outsourcing is the process of hiring a third-party provider to convert patient care records into standardized codes. Like physician notes, lab results, and diagnostic reports, are converted into standardized billing codes.
These providers employ certified coders (e.g., CPC, CCS) who work remotely using secure, HIPAA-compliant systems. Their services typically include reviewing documentation, assigning
codes, ensuring quality, and submitting claims electronically to insurers.
Key Benefits of Medical Coding Outsourcing
Outsourcing medical coding is no longer just about saving costs; it’s a strategic approach that boosts efficiency, ensures compliance, and strengthens the revenue cycle.
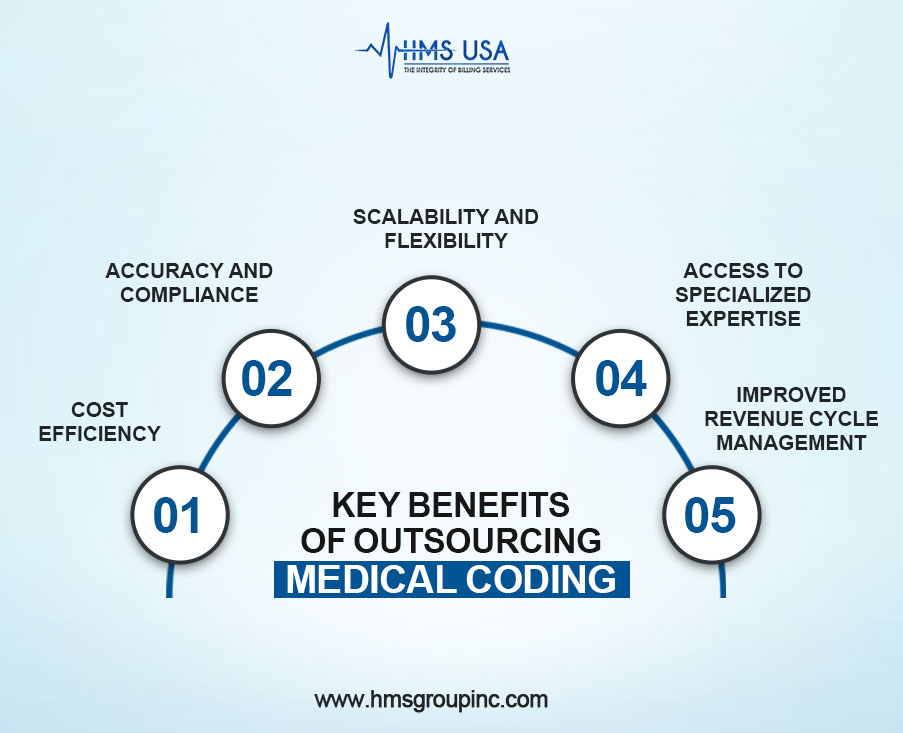
Here are the key benefits of partnering with professional medical coding services:
- Cost Efficiency
Outsourcing reduces costs associated with hiring, training, benefits, office space, and ongoing education.
For instance, a mid-sized clinic reduced its administrative overhead by 35% in the first year, reinvesting the savings into patient care and IT upgrades.
- Accuracy and Compliance
Certified coders bring expert knowledge in CPT, ICD, and HCPCS coding, reducing claim denials and audit risks. Consistent quality control improves accuracy and documentation standards.
- Scalability and Flexibility
Outsourcing enables the quick scaling of coding resources to meet changes in patient volume or specialty expansions. Many providers offer 24/7 support, ensuring uninterrupted revenue cycles across time zones and holidays.
- Access to Specialized Expertise
Outsourced coders are trained in diverse specialties (e.g., cardiology, orthopedics), enhancing documentation quality for proper reimbursement. They stay updated on industry changes to reduce denials and improve claim acceptance.
- Improved Revenue Cycle Management
Accurate coding speeds up claim submissions, reduces delays and denials, and accelerates reimbursements. When combined with billing services, outsourcing results in streamlined workflows and enhanced financial outcomes.
Role of Medical Coding Outsourcing Companies
Medical Billing coding companies boost accuracy, productivity, and compliance by providing skilled coders trained in multiple specialties and up-to-date coding guidelines. They offer analytics to identify trends, reduce denials, and improve revenue cycles. Many also utilize advanced technologies, such as AI-assisted coding and robotic process automation, for faster and more accurate results.
Differentiating In-House vs. Outsourced Coding and Billing Services
- Cost-effectiveness: Outsourcing reduces costs associated with hiring, training, and infrastructure.
- Expertise access: Specialized coders ensure high accuracy across multiple disciplines.
- Scalability: Providers can adjust coding volume based on patient load or seasonal variations.
- Compliance assurance: Outsourcing firms stay current with evolving coding regulations and payer requirements.
The Impact of Medical Coding Outsourcing on Patient Care
Outsourcing medical coding has become a strategic move for many healthcare providers, positively impacting patient care and outcomes.
By delegating coding tasks to specialized experts, providers ensure higher accuracy and compliance, which directly supports better clinical documentation and billing processes. Accurate coding translates into clearer patient records, enabling clinicians to make more informed decisions based on comprehensive data.
How Accurate Coding Supports Better Clinical Decision-Making
Accurate medical coding ensures that patient information is correctly documented and easily accessible. This precision enables healthcare providers to track diagnoses, treatments, and outcomes effectively, thereby reducing errors and enhancing care quality.
When codes accurately reflect patient conditions and procedures, clinicians can rely on consistent data to tailor treatments, monitor progress, and avoid unnecessary interventions.
Reducing Administrative Burden to Improve Provider-Patient Interactions
Outsourcing coding reduces the administrative workload on healthcare staff, freeing up valuable time for direct patient care.
Providers spend less time on paperwork and billing issues, allowing them to focus more on patient interaction and personalized treatment. This shift enhances communication, builds stronger patient relationships, and ultimately leads to improved satisfaction and health outcomes.
Industry Trends in 2025 Driving Outsourcing
In 2025, the healthcare sector is undergoing rapid changes due to the introduction of new technologies, evolving regulations, and the growing need to meet patient needs. This is leading to more medical coding and billing being done by third-party organisations.
Growing Specialty Care Needs
As specialties like cardiology and oncology expand, outsourcing provides access to expert coders who ensure accurate, complex coding aligned with specific procedures.
Faster Reimbursement Cycles
With tighter financial margins, providers rely on outsourced services to reduce errors and speed up claims processing, resulting in quicker reimbursements and improved cash flow.
AI and Automation Integration
Medical billing services companies are adopting AI and robotic process automation to boost coding accuracy, minimize manual errors, and efficiently handle large claim volumes, thereby enhancing productivity.
Regulatory Compliance
Outsourcing helps healthcare providers stay compliant with evolving regulations, such as ICD-11 and HIPAA, by utilizing specialists trained in the latest requirements, thereby reducing legal risks.
How to Choose the Right Medical Coding Outsourcing Companies/ Partner
Factors To Consider:
- Certification and Expertise
- Technology and Integration
- Average Turnaround Time
- Assess average turnaround time for coding submissions.
- HIPAA Compliance and Data Security
Key Questions to Ask Medical Coding Outsourcing Companies
- What certifications do your coders have?
- How do you ensure coding accuracy and reduce errors?
- Which coding technologies and platforms are used?
- How do you manage high-volume coding demands?
- Can you provide client references or case studies?
Final Thoughts
Outsourcing medical coding enhances accuracy, streamlines reimbursements, reduces costs, and ensures compliance with evolving regulations. Trends like AI-assisted coding, predictive analytics, and global talent are reshaping the field.
Partnering with a trusted coding provider enables healthcare organizations to focus on patient care while enhancing efficiency, financial stability, and regulatory compliance.
Selecting a reliable partner to outsource medical coding represents an investment in the future of your practice. Look at how outsourcing could speed up your processes and boost your bottom line.
To arrange a free consultation or obtain our thorough guide on best practices in medical coding outsourcing services, contact HMS Group Inc. right now. With HMS Group Inc., start towards scalable, compliant, and effective medical coding solutions.











