Healthcare is changing fast with smarter technology, shifting regulations, and a stronger push for patient-first care. But one thing remains constant: medical billing and coding are still at the heart of getting paid accurately and staying compliant.
Did you know that nearly 25% of hospital costs in the U.S. come from administrative tasks like billing? Or that over 90% of healthcare providers are now using automation to improve their revenue cycle? These results show just how critical it is to keep up with the latest trends.
In this blog, we’ll take you inside the future of medical billing and coding. From AI-powered tools to unmatchable digital systems, discover how innovation is transforming the way healthcare organizations handle billing, compliance, and cash flow.
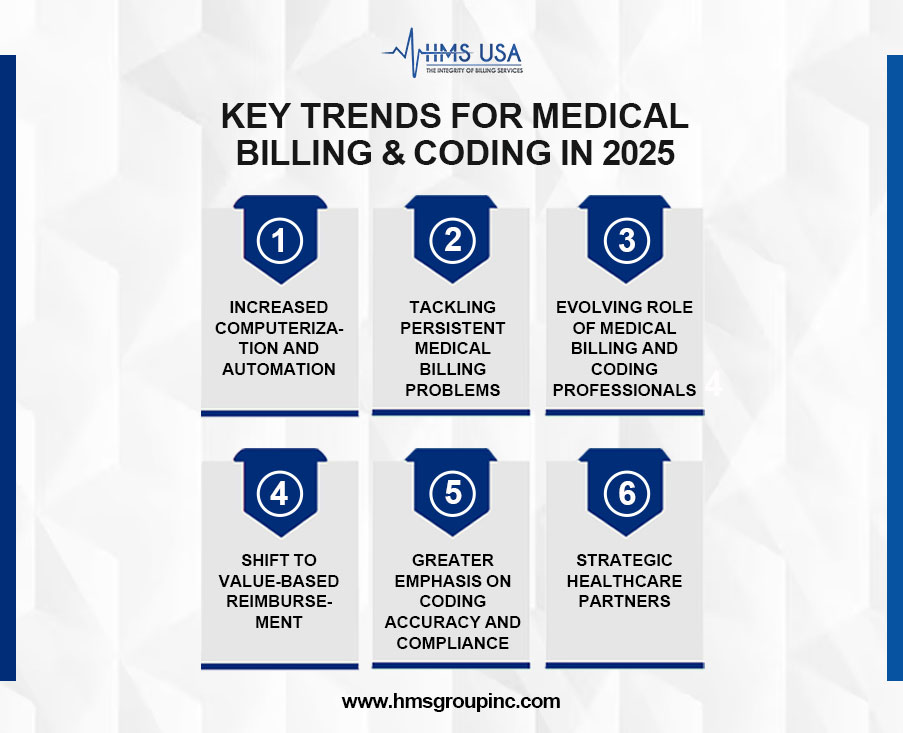
Trend #1: Increased Computerization and Automation
One of the key trends reshaping medical billing and coding is the rapid adoption of automation and computerization of medical billing and coding. Technologies like AI and machine learning enhance coding accuracy by analyzing clinical data and suggesting appropriate codes, helping reduce claim denials and audits.
The integration of electronic health records (EHRs) with billing systems also streamlines workflows, cuts manual data entry, and ensures accurate, up-to-date coding based on complete patient information.
Automation boosts operational efficiency by handling repetitive tasks, allowing staff to focus on compliance and patient care. It also minimizes common coding errors, such as incorrect modifiers or mismatched diagnoses.
Automation is no longer optional; it’s essential for efficient, accurate medical billing and coding in 2025 and beyond.
Trend #2: Tackling Persistent Medical Billing Problems
Despite technological progress, healthcare providers still face persistent billing challenges such as claim denials, payment delays, inaccurate coding, and complex compliance rules. According to the MGMA, denial rates in medical practices average 5–10%, often due to coding errors or missing data. Navigating varied insurance policies only adds to the complexity.
To combat these issues, providers are adopting automation and advanced analytics. Tools like automated claim scrubbing and predictive analytics help catch errors early, reduce denials, and improve revenue cycle management.
New technologies simplify insurance eligibility and verification. Real-time insurer contact with integrated billing platforms speeds claims and reduces rejections. These improvements are essential to fixing medical billing inefficiencies.
Trend #3: Evolving Role of Medical Billing and Coding Professionals
By 2025, medical billing and coding professionals will no longer just be data processors—they will be strategic contributors to healthcare systems. Employers now seek candidates with hybrid skills in data analytics, regulatory compliance, and healthcare IT.
The role is shifting from basic documentation to optimizing data for value-based care, quality reporting, and population health goals. Coders must ensure accuracy, compliance, and meaningful use of clinical data.
To stay competitive, professionals must continuously update their skills through training, certifications, and cross-functional learning. Proficiency in AI-driven coding tools, EHRs, and regulations is now essential.
Trend #4: Shift to Value-Based Reimbursement
A key trend in medical billing and coding is the shift from fee-for-service to value-based reimbursement, which focuses on patient outcomes, care quality, and cost efficiency. Models like ACOs, bundled payments, and pay-for-performance demand more precise and holistic coding.
This shift requires coders to ensure accurate documentation that reflects social determinants of health (SDoH), risk adjustment, and care coordination. Data-driven coding—powered by integrated EHRs and billing systems—supports timely, accurate reporting aligned with quality metrics. Ultimately, this transition helps improve care delivery while maintaining financial sustainability.
Trent #5: Greater Emphasis on Coding Accuracy and Compliance
In 2025, coding accuracy and compliance are more critical than ever. The adoption of ICD-11 and updated CPT codes demands greater precision in documenting and billing diagnoses and procedures. These changes aim to boost clinical specificity, streamline reporting, and align with global standards.
However, common errors—like upcoding, undercoding, and incorrect modifier use—remain widespread, leading to claim denials, audits, and financial penalties. As regulatory scrutiny intensifies, healthcare organizations must strengthen audits, quality checks, and coder training.
The need for certified, well-trained coders who can accurately interpret complex documentation is rising. With reimbursement closely tied to compliance, coding accuracy is now a non-negotiable priority for providers.
Trend #6: Medical Billing and Coding Professionals as Strategic Healthcare Partners
In 2025, medical billing and coding professionals are evolving from data entry roles to key strategic contributors. Employers are now seeking individuals with extensive knowledge of IT systems, healthcare regulations, and data analytics.
The focus has shifted from simple documentation to leveraging data for compliance, value-based care, and population health management. Coders must ensure that clinical data accurately reflects care quality and supports organizational goals.
To remain competitive, professionals must pursue ongoing education and master AI tools, EHR integration, and regulatory compliance.
Avoidable Mistakes in Medical Coding – Common Medical Coding Mistakes
Medical coding errors can lead to claim denials, delayed reimbursements, and compliance issues.
Here are some of the most common mistakes:
- Incorrect or Incomplete Codes
Using outdated, incorrect, or incomplete ICD, CPT, or HCPCS codes is a frequent issue. This often stems from a lack of updates or insufficient training.
- Upcoding or Undercoding
Assigning codes that reflect a higher or lower level of service than provided can trigger audits and impact revenue integrity.
- Missing Modifiers
Omitting necessary modifiers or using them incorrectly can result in denied or misprocessed claims.
- Improper Documentation
Inaccurate or insufficient clinical documentation makes it hard to justify codes, leading to billing errors and compliance risks.
- Unbundling Services
Separating services that should be billed together as a bundle can violate payer rules and result in penalties.
Avoiding these common mistakes requires continuous training, thorough audits, and close collaboration between providers and coding professionals.
Final Words
Medical billing and coding are shifting quickly because of automation, value-based care, stricter rules about compliance, and changes in the positions of professionals.
To stay competitive and compliant in 2025 and beyond, healthcare providers must innovate, upskill, and prioritize data accuracy. In line with the continuously shifting goal of medical billing and coding to ensure efficiency, accuracy, and improved patient outcomes.
Collaborate with HMS Group Inc. to get expert advice and billing, coding, and compliance solutions that are ready for the future. Getting a successful start with the right help.