Medical billing denials are a common problem for healthcare providers. They slow down payments, create extra paperwork, and can even lead to lost revenue if not fixed quickly.
One of the most common denials is the CO-18 Denial Code. This happens when a claim is denied because it appears to be a duplicate submission. For billing staff and providers, knowing how to handle this denial is essential for keeping payments on track.
In this blog, we’ll explain the leading causes of CO-18 denials, how to fix them, and what steps you can take to prevent them in the future.
What Is Denial Code CO-18 Denial?
CO-18 Denial Code Description
The Denial code CO-18 means the insurance company has rejected a claim because it looks like a duplicate. This happens when a claim for the same patient, provider, service, and date has already been received and processed.
What Are Duplicate Claim Denials?
A duplicate claim in medical billing means the same claim (or one that looks almost the same) is sent more than once. This can happen by mistake during resubmission, due to system errors, or because of poor communication between providers and billing staff. Since billing is complex and involves many steps, CO-18 is one of the most common denial codes. Even slight differences in details like dates or procedure codes can cause a denial.
Common Reasons for CO-18 Denials – CO-18 Denial Code Reason
Resubmitting without corrections: If a claim is sent again without fixing the original error, the payer’s system marks it as a duplicate.
System or clearinghouse errors: Technical problems may accidentally send the same claim multiple times.
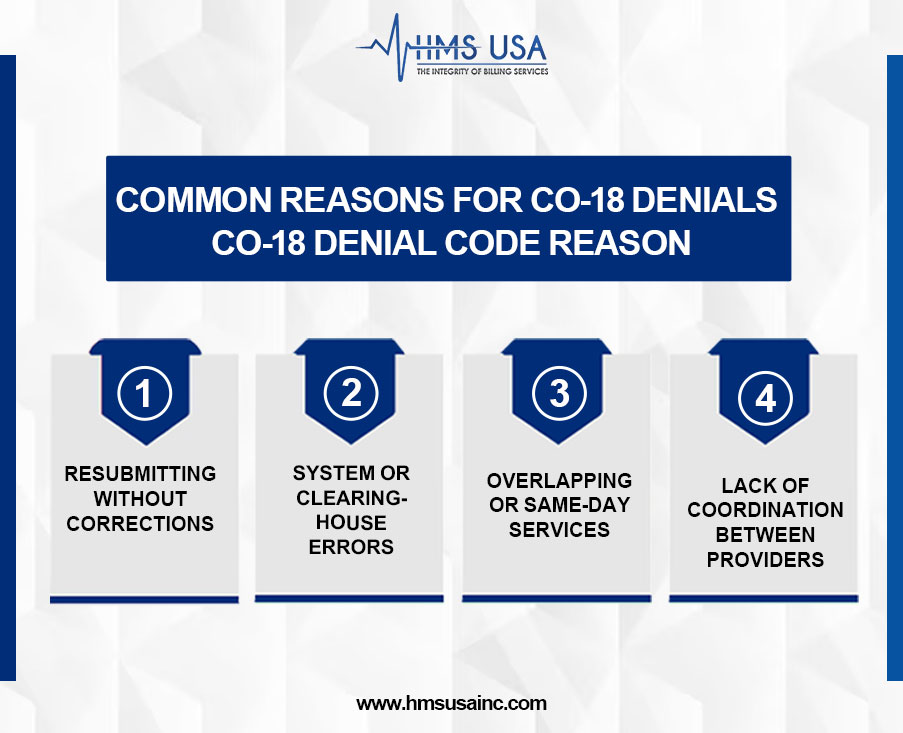
Overlapping or same-day services: When multiple services for the same patient on the same day look similar, the system may treat them as duplicates even if they are valid.
Lack of coordination between providers: Different providers or departments may bill for the same or similar services without realizing it, leading to duplicate submissions.
Why CO-18 Denials Happen and How They Impact Practices
CO-18 denials occur when an insurance payer rejects a claim as a duplicate. This usually happens if the same service for the same patient, on the same date, has already been billed by the same provider.
Common causes include resubmitting a claim without making necessary corrections, system or clearinghouse errors that lead to multiple submissions, and overlapping services billed on the same day.
1. Delays in Payment
When a claim is denied as a duplicate (CO-18), payment gets held up until the issue is fixed. This can slow down cash flow, which many practices depend on.
2. Extra Work for Billing Teams
Staff must spend time finding the error, correcting it, and resubmitting the claim. This takes focus away from other essential billing tasks and slows the entire revenue cycle.
3. Why Finding the Cause Quickly Matters
It’s essential to quickly determine why the claim was denied, whether it’s due to a system error, a repeated submission, or overlapping services. Fixing the issue quickly helps avoid future denials and keeps revenue flowing smoothly.
How to Fix CO-18 Denials
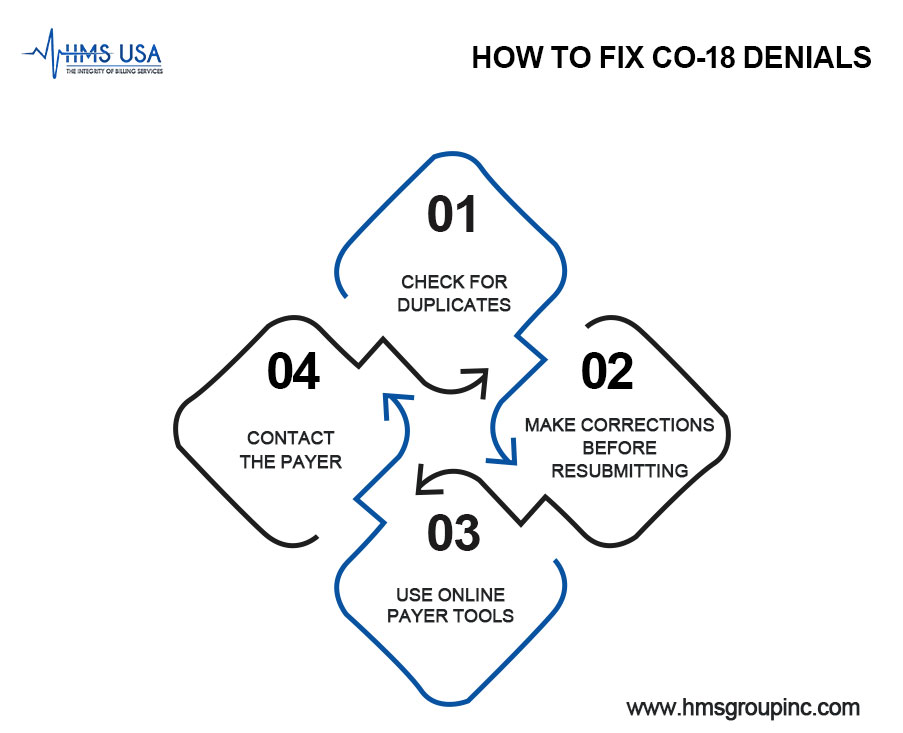
- Check for Duplicates: Review claim history in your billing system and the payer’s records.
- Make Corrections Before Resubmitting: Don’t send the same claim again without fixing errors, or it will just get denied again.
- Use Online Payer Tools: Many payers offer portals that allow you to view the reason a claim was marked as a duplicate.
- Contact the Payer: If it’s still unclear, reach out to the payer directly for clarification.
How to Prevent Duplicate Claim Denials
- Use Advanced Billing Software: Claim scrubbing tools can catch errors and duplicates before you submit.
- Train Your Staff: Ensure billing teams understand the proper submission steps, including checking claim status first.
- Track Claims in Real Time: Claim tracking systems let you monitor progress and avoid unnecessary resubmissions.
- Stay in Touch with Payers: Good communication helps clear up issues quickly and reduces repeat problems.
Final Thoughts!
The CO-18 denial code happens when a claim is marked as a duplicate. This is one of the most common issues in medical billing. By checking claim history, fixing mistakes, and staying in touch with payers, providers can resolve these denials. Even better, taking preventive steps like training staff, using claim-scrubbing software, and tracking claims carefully can stop many denials before they happen. This saves time, reduces stress, and helps practices get paid faster.
Duplicate claim denials slow down payments and hurt cash flow. Now is the right time to review your billing process and improve your denial management strategy. For expert help with reducing CO-18 denials and keeping your revenue cycle running smoothly, contact HMS Group Inc. today.
Duplicate claim denials slow down payments and damage cash flow. This is the ideal moment to enhance your denial management approach and evaluate your billing procedure.
For expert help with reducing CO-18 denials and keeping your revenue cycle running smoothly, contact HMS Group Inc. today.
FAQs
What does the CO-18 denial code mean?
The CO-18 denial code means your claim was denied because the insurance company thinks it’s a duplicate of one already submitted. In simple words, they believe the same claim was sent more than once.
Why do duplicate claim denials (CO-18) happen?
This usually happens if the same claim is sent again without changes, if services overlap on the same day, or if there’s a mistake in the billing system.
How can I fix a CO-18 denial code?
Check the claim history first to see if it was already submitted. If yes, don’t resend it. If corrections are needed, update the claim before resubmitting. You can also call the insurance payer to confirm the claim status.
How can providers avoid CO-18 duplicate claim denials?
Prevention is better than fixing. Providers can use billing software to catch errors, train staff to avoid resubmitting claims by mistake, and keep track of claim statuses through payer portals.
Does a CO-18 denial slow down payments?
Yes. When claims are denied as duplicates, payments are delayed, and staff spend extra time resolving the issue. Preventing CO-18 denials helps providers get paid faster and keeps billing smoother.