Chronic conditions like diabetes, heart disease, and respiratory issues are becoming more common, affecting millions worldwide. These long-term health challenges not only impact patients’ quality of life but also put a strain on healthcare systems, leading to higher costs and more hospital visits. For example, over 40% of adults in the U.S. live with at least one chronic condition, and more than 1 in 4 adults suffer from multiple chronic diseases.
But there’s hope! Chronic Care Management (CCM) offers a smarter, more coordinated approach to managing these conditions. With CCM, patients get the support they need to stay healthier, avoid complications, and reduce hospitalizations, while healthcare providers can deliver more effective care.
What is Chronic Care Management?
Chronic Care Management (CCM) is a healthcare service focused on the long-term management of chronic health conditions. The purpose of CCM is to provide patients with personalized care plans that are tailored to their specific health needs. This type of care involves continuous monitoring, regular follow-ups, medication management, and the coordination of services to prevent the worsening of chronic conditions.
Chronic diseases account for 7 out of 10 deaths in the U.S. and are responsible for 75% of healthcare spending.
The main goal of CCM is to improve the overall health and quality of life for individuals with chronic conditions. It involves a patient-centered approach, wherein healthcare professionals work together to ensure that patients receive the care they need to manage their conditions and maintain their independence.
Who Qualifies for CCM Services?
CCM services are generally available to individuals who suffer from at least one chronic condition that has been ongoing or is expected to last for a year or more.
These may include conditions such as asthma, diabetes, hypertension, heart disease, chronic obstructive pulmonary disease (COPD), and many others.
However, eligibility may be different based on the healthcare provider and the program’s rules.
Patients typically need at least two visits to their healthcare provider within the past year to qualify for CCM services. The provider must also determine that ongoing management and monitoring are necessary to prevent complications.
Benefits to Patients and Providers
Chronic Care Management (CCM) benefits both patients and healthcare providers. For patients, it offers a structured approach to managing chronic conditions, improving health outcomes, quality of life, and reducing hospitalizations. Patients gain the knowledge and tools to better manage their health.
For providers, CCM enhances care efficiency by enabling continuous monitoring and early issue detection, reducing hospital visits, and improving patient satisfaction. Additionally, it helps lower healthcare costs by preventing complications and costly treatments.
Chronic Care Management CPT Codes
Chronic Care Management (CCM) is essential for patients with multiple chronic conditions requiring ongoing care. Healthcare providers use specific CPT codes to ensure proper reimbursement for CCM services.
Commonly Used Chronic Care Management CPT Codes:
CPT 99490: Covers non-face-to-face care for patients with two or more chronic conditions, involving at least 20 minutes per month of medication management and care coordination.
CPT 99439: A newer code for comprehensive care, including telehealth and remote monitoring, used for patients with higher or more complex care needs.
CPT 99439 (alternative): For patients with multiple chronic conditions requiring extensive care management beyond standard CCM services.
Medicare and CCM – Reimbursement and Guidelines
CCM Medicare covers Chronic Care Management (CCM) services under Part B for eligible patients with two or more chronic conditions that are expected to last at least 12 months or until death. These conditions must cause significant functional limitations and require involvement from multiple healthcare providers.
CCM services aim to improve care coordination, reduce hospital admissions, and encourage patient self-management. To receive reimbursement, providers must meet strict eligibility and documentation requirements.
Required components for reimbursement:
- Comprehensive care plan: Updated regularly, detailing chronic conditions, treatment goals, and care coordination.
- Patient consent: Explicit consent must be documented before initiating care.
- 24/7 access to care: Providers must ensure patients have access to urgent care services at any time.
- Care coordination: Providers must document coordination with other healthcare providers, including specialists and pharmacists.
- CMS compliance and documentation standards:
- Detailed documentation: All care coordination, patient communications, and management time must be recorded.
- Accurate coding: Providers must use the correct CPT code based on care complexity and time spent.
- Regular updates: The care plan must be updated to reflect any changes in the patient’s condition or treatment plan.
- HIPAA compliance: Ensure patient information is protected according to privacy and security regulations.
Chronic Care Management Codes and Billing Process
Chronic Care Management (CCM) codes allow healthcare providers to receive reimbursement for managing patients with chronic conditions. Proper usage ensures accurate reimbursement and high-quality care.
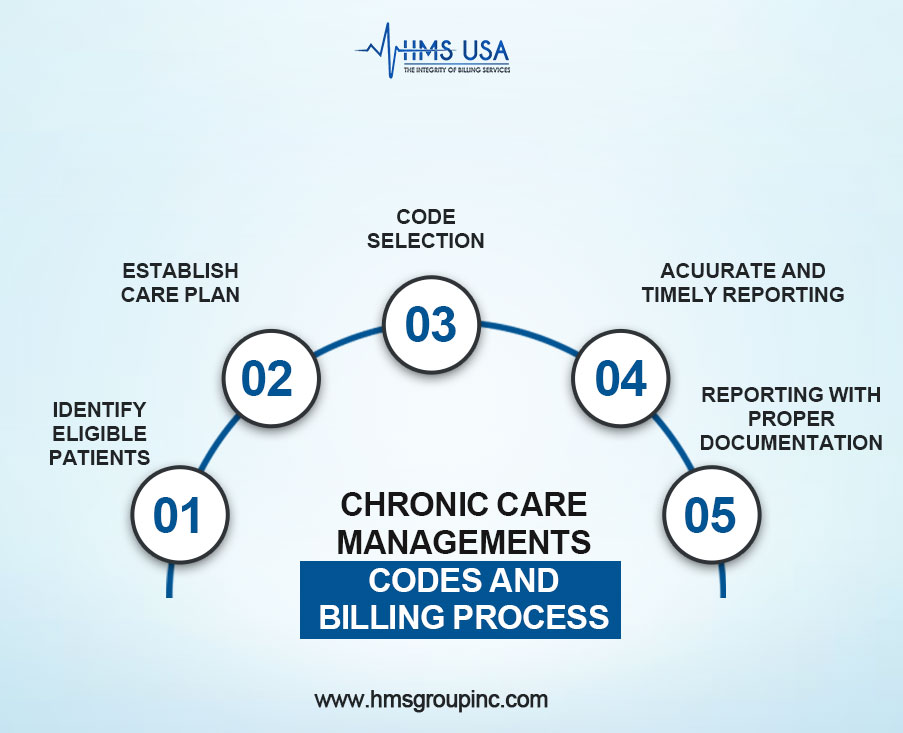
Step-by-Step CCM Code Usage
1. Identify Eligible Patients
CCM codes apply to patients with two or more chronic conditions expected to last at least 12 months, significantly impacting health.
2. Establish Care Plan
Providers must develop a comprehensive care plan, including medication management, lifestyle changes, and regular monitoring. This plan must be well-documented and updated.
3. Code Selection
CPT Code 99490: For 20+ minutes of non-face-to-face care coordination.
CPT Code 99439: For more complex care requiring higher management.
4. Report Time Accurately
Document cumulative time spent on care coordination over the month. Non-face-to-face interactions like phone calls and emails count toward total time.
5. Proper Documentation and Reporting
Accurate documentation of patient interactions and care updates is important for reimbursement. Failure to document correctly can result in claim denials
Benefits of Implementing CCM in Medical Practice
- Proactive management and continuous monitoring of chronic conditions lead to fewer hospitalizations.
- Better long-term health outcomes through consistent adherence to treatment plans.
- Enhanced quality of life for patients with regular follow-ups and care coordination.
- Reimbursement opportunities through CCM codes help offset costs and improve financial sustainability.
- Stronger patient-provider relationships are built through frequent communication and support.
- Increased patient engagement and satisfaction as providers actively manage their health.
Concluding Thoughts!
Chronic Care Management (CCM) is important for managing the rising number of people with chronic conditions, making long-term care more efficient, and better patient outcomes.
CCM makes sure that patients get the best care possible by providing ongoing support, tracking, and individualized care.
Healthcare providers have to constantly evaluate and adjust their Chronic Care Management (CCM) billing methods to comply with changing standards and optimize compensation. HMS Group Inc. helps practices by:
- Optimizing CCM service integration.
- Following current billing codes and norms.
- Strategic billing maximizes reimbursement.
- Offering a free CCM billing audit to find improvements.
- Enhancing your practice’s financial outcomes.
Contact HMS Group Inc. today to schedule your free audit and take the next step in delivering exceptional care while improving your practice’s financial success.








