
Top Common Internal Medicine CPT Codes in 2025
CPT coding may seem like just numbers and paperwork, but for internal medicine practices, it’s the backbone of accurate payment and compliance. These codes, maintained by the American Medical Association (AMA), help standardize the reporting of medical services so that insurers understand exactly what care was provided.
In 2025, staying on top of CPT code updates is more important than ever. With ongoing changes in telehealth, preventive care, and chronic disease management, even minor coding errors can result in denied claims, reduced reimbursements, and compliance issues.
Getting CPT coding right doesn’t just protect your bottom line; it also ensures accurate reimbursement. Your documentation tells the full story of the care you deliver. In a world moving toward value-based care, precise coding is more than a necessity—it’s a strategy for success.
What Are Internal Medicine CPT Codes?
CPT (Current Procedural Terminology) codes are standardized numeric identifiers used by healthcare providers to describe medical procedures and services for billing purposes across private insurers, Medicare, and Medicaid.
In internal medicine, these codes are essential due to the specialty’s broad and complex scope. Internists manage multiple comorbidities, often requiring diverse evaluation and management (E/M) services, diagnostics, and preventive care.
Unlike procedure-heavy surgical specialties, internal medicine focuses on cognitive services, chronic disease management, and care coordination, making precise E/M coding critical.
Why CPT Coding Matters for Internal Medicine Practices
In internal medicine, CPT coding is crucial for accurate billing, ensuring timely payment, and adhering to regulations. Claim denials, payment delays, and audits can be avoided by using correct coding. This ensures steady income and efficient billing.
It also ensures that medical records accurately reflect care, which helps with legal protection, effective reporting, and compliance with regulations such as those from CMS. Correct coding leads to greater transparency and improved outcomes for patients.
Challenges Commonly Faced in Internal Medicine Billing
Billing for internal medicine encompasses a wide range of services, including regular visits, managing chronic diseases, and making diagnoses. This increases the likelihood of coding mistakes occurring.
Common challenges include:
- Under-coding or over-coding due to ambiguous documentation.
- Staying updated with annual CPT code changes.
- Distinguishing between similar codes, especially in Evaluation and Management (E/M) categories.
- Managing chronic care and preventive services, which often have nuanced billing guidelines.
- Ensuring coordination between billing staff and clinicians for accurate code selection.
Top CPT Codes Used in Internal Medicine (2025)
Internal medicine relies on a core set of Common CPT Codes For Internal Medicine for common services. Keeping up to date with changes is essential for compliance and revenue optimization.
Evaluation and Management (E/M) Codes
E/M codes cover office visits, consultations, and hospital care:
- 99213: Established patient visit, 20–29 minutes.
- 99214: Established patient visit, 30–39 minutes, moderate Complexity.
Documentation must support the billed complexity, reflecting the time and medical decision-making involved.
Preventive Care and Wellness Visits
Used for routine wellness exams, typically covered by insurance:
- 99396: Preventive visit for patients 40–64 years.
- 99397: Preventive visit for patients 65 and older.
These differ from E/M visits, as they focus on prevention rather than treating complaints.
Chronic Care Management (CCM)
Vital in value-based care:
99490: CCM with ≥20 minutes of clinical staff time per month.
99487: Complex CCM with ≥60 minutes and moderate-to-high complexity.
Documentation must include care planning, patient consent, and time spent.
Procedures and In-Office Diagnostics
Common codes include:
- 93000: ECG with interpretation.
- 36415: Venipuncture blood collection.
- 96372: Therapeutic or diagnostic injection.
Accurate documentation and adherence to frequency limits are necessary to avoid denials.
Updates or Changes in 2025 Coding Guidelines
The 2025 CPT code set features minor updates to E/M guidelines and new guidance on digital health services, including:
- Clarified time-based coding for prolonged services
- New add-on codes for remote therapeutic monitoring and digital patient engagement
- Revised CCM code language for clearer documentation
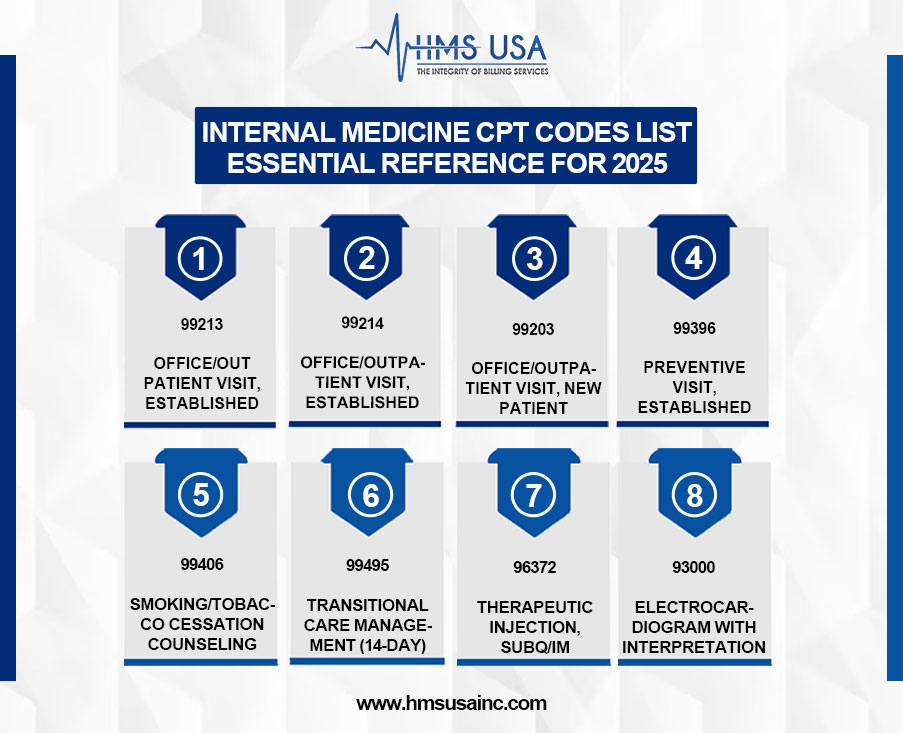
Internal Medicine CPT Codes List – Essential Reference for 2025
| CPT Code | Description | Typical Use-Case | Documentation Tips |
|---|---|---|---|
| 99213 | Office/outpatient visit, established | Moderate complexity visit for follow-up or chronic condition | Document patient history, assessment, and time spent |
| 99214 | Office/outpatient visit, established | Comprehensive exam and management of multiple issues | Include MDM level and treatment changes |
| 99203 | Office/outpatient visit, new patient | New patient with moderate issues | Detail the chief complaint, new diagnosis, and complexity |
| 99396 | Preventive visit, established (age 40–64) | Annual wellness check-up | Include risk factors and screenings performed |
| 99406 | Smoking/tobacco cessation counseling (3–10 min) | Brief intervention during a regular visit | Specify the duration of counseling and advice given |
| 99495 | Transitional Care Management (14-day) | Follow-up after hospital discharge | Document communication with the patient and medication review |
| 96372 | Therapeutic injection, subq/IM | Administering injections (e.g., B12, vaccines) | Include medication, dose, and site of injection |
| 93000 | Electrocardiogram with interpretation | Evaluating cardiac symptoms or routine screening | Attach EKG tracing and interpretation summary |
Differences Between Primary Care CPT Codes and Internal Medicine Codes
Overlap
- Both use standard E/M codes (e.g., 99213–99215).
- Preventive services, vaccinations, and basic counseling codes apply to both.
Differences
- Internal medicine manages more complex, chronic, and multisystem conditions (e.g., heart failure, diabetes, COPD).
- It commonly uses codes for advanced diagnostics, such as cardiac testing (94010) and chronic care management (99490).
Key Internal Medicine Procedure Codes
- 99487 – Complex chronic care management
- 94640 – Nebulizer treatment
- 36415 – Routine venipuncture
Concluding Thoughts
Compliance, proper invoicing, and effective revenue cycle management all depend on mastery of the 2025 Internal Medicine CPT codes. To lower denials, stay current on CMS and AMA changes, educate staff on documentation and modifiers, and align coding with clinical processes.
Proper CPT safeguards revenue and boosts clinical and operational performance. Bookmark or download the CPT code list for quick access. For expert support, consult billing professionals or use smart billing software to reduce errors and accelerate reimbursements.
Need professional guidance settling internal medicine billing complexity?
Contact HMS Group Inc. today for customized support in coding, claims, and compliance. Visit our website or call us to learn more about how we can optimize your medical billing workflow.


