Ever wondered what helps your doctor’s office run smoothly and your insurance claims get approved without delays? The answer is often something called medical credentialing.
In simple terms, credentialing is a detailed check of a healthcare provider’s education, licenses, experience, and background. It makes sure they’re fully qualified to give safe, legal, and reliable care. There are different types of credentialing in medical billing, and each serves an important purpose, like keeping billing accurate and making sure providers get paid on time. Without it, payments can be delayed, claims denied, or providers may not be able to treat certain patients.
Credentialing isn’t just paperwork. It builds patient trust, keeps healthcare organizations following the rules, reduces risks, and helps a practice stay financially healthy.
In this blog, we are going to discuss the different types of medical credentialing, credentialing in healthcare, and how each type of credentialing plays an important role in healthcare.
What is Medical Credentialing?
Medical credentialing is the process of checking a healthcare provider’s qualifications to make sure they meet the standards needed to care for patients safely and effectively.
It includes:
- Confirming qualifications and licenses: Making sure degrees, certifications, and state licenses are valid and up to date.
- Reviewing work history: Looking at past jobs, malpractice claims, and any disciplinary actions.
- Ensuring ongoing skills: Checking that the provider continues training and keeps their skills current.
Credentialing is also important for billing. Insurance companies require providers to be credentialed before they will pay for claims. Without it, payments can be delayed or denied, causing financial losses. In short, credentialing protects both patient safety and the financial stability of healthcare organizations.
The Credentialing Process: Step-by-Step
Here Is a Step-by-Step Guide:
1. Gathering Documents and Licenses
The process starts with collecting important papers like medical licenses, board certifications, malpractice insurance, DEA registration (if needed), work history, and references. These must be correct and up to date to avoid delays.
2. Primary Source Verification (PSV)
Next, the credentialing team double-checks these documents with sources such as licensing boards, schools, or certification agencies to make sure everything is valid and meets state and national standards.
3. Final Approval and Re-Credentialing
After everything is verified, the provider is approved to work or join insurance networks. Credentialing isn’t done just once; it usually needs to be renewed every 2–3 years to make sure providers still meet all requirements.
Types of Medical Credentialing
Medical credentialing is how healthcare organizations check that providers and related companies are qualified, follow the rules, and can be trusted. Each type of credentialing plays a role in keeping patients safe, meeting legal requirements, and running healthcare smoothly.
1. Provider Credentialing
This is when a provider’s education, training, licenses, and work history are reviewed to make sure they are qualified to give safe, effective care. It’s required before joining an insurance network so the provider can bill for services. Without it, insurance claims may be denied.
The process also helps keep patient trust by making sure healthcare providers meet important national and state rules. Besides checking their qualifications, provider credentialing can include background checks, talking to references, and ongoing reviews to ensure the provider continues to follow all the rules and stays qualified over time.
2. Hospital Credentialing
Hospitals use this process to decide which doctors and other medical staff can work in their facilities. They check licenses, certifications, malpractice history, and policy compliance. Regulators like The Joint Commission require it, and providers must go through it regularly to stay approved.
Hospital credentialing also includes reviewing a provider’s clinical privileges. The specific treatments or procedures they are allowed to perform are based on their training and experience. This step helps make sure providers only offer care they are qualified for. By doing this, hospitals protect patient safety, follow their standards, and keep their accreditation in good standing.
3. Payer Credentialing
This is how providers get approved by insurance companies to treat their members. It involves sending documents, verifying qualifications, and signing agreements. Without payer credentialing, providers can’t get paid by insurers.
This method makes sure providers meet an insurance company’s standards and that patients get care from qualified professionals in the insurer’s network. Because each insurance company has its own rules, providers often have to go through a separate credentialing process for every company they work with.
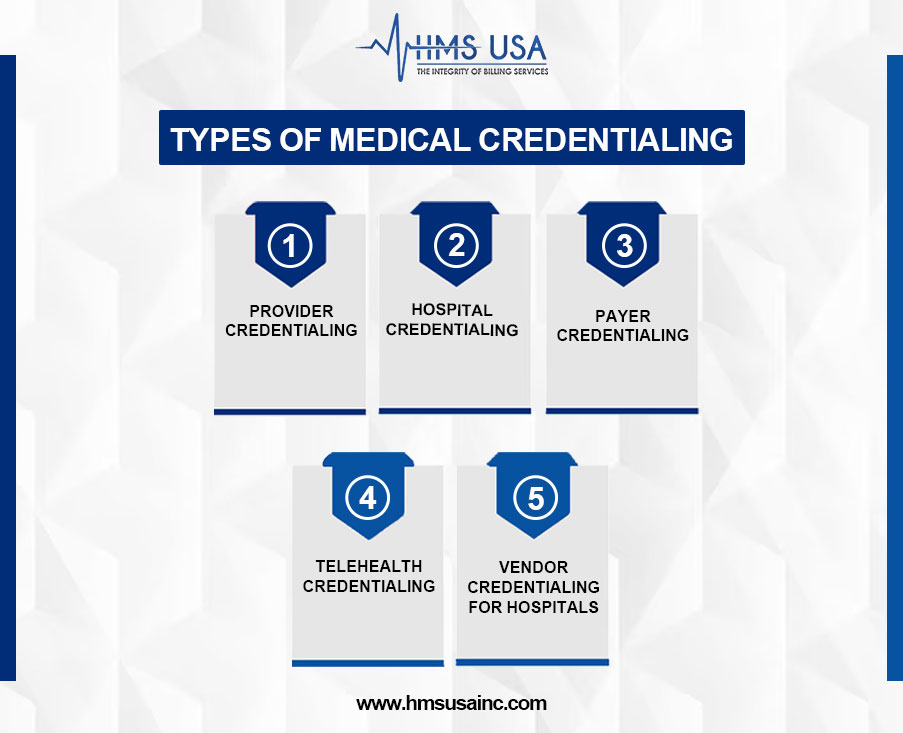
4. Telehealth Credentialing
For providers offering virtual care, this ensures they are licensed in the patient’s state and follow telehealth laws. Rules vary by state, so this process helps maintain quality care and avoid legal issues.
Telehealth credentialing makes sure a provider uses safe and secure technology, follows privacy rules like HIPAA, and meets telemedicine guidelines. As more people turn to virtual care, this process helps keep patients, providers, and healthcare organizations safe from legal and compliance problems.
5. Vendor Credentialing for Hospitals
Hospitals also check outside companies they work with, like medical equipment suppliers or cleaning services, to make sure they follow important safety rules. They do background checks to see if these companies are trustworthy.
Hospitals ask for proof that the companies have insurance, which helps protect everyone if something goes wrong.
They also make sure these companies follow infection control steps to keep patients and staff safe from germs. Checking these vendors carefully helps the hospital stay safe and healthy for everyone.
Common Challenges in Credentialing & How to Overcome Them
Credentialing is important for healthcare providers, but it can be slow and frustrating if certain problems aren’t handled early.
- Delays in Processing: The process can take 2–4 months, sometimes longer, if verification sources respond slowly or if applications are incomplete.
Solution: Start early, ideally 3–4 months before a provider’s start date, and check in regularly with the organizations handling your application.
- Incomplete Paperwork: Missing or outdated licenses, expired insurance, or incorrect work history can cause major delays.
Solution: Keep all licenses, certifications, and insurance details in one organized place, and review them regularly to make sure they’re up to date.
- Different Rules for Different Payers: Every insurance company may have its forms, timelines, and requirements.
Solution: Work with a credentialing expert or use software that helps you manage multiple applications at once to save time and avoid mistakes.
Why Timely Credentialing Matters for Healthcare Providers
Getting credentialed on time keeps your revenue on track. If you’re not credentialed, insurance companies can delay or deny payment for your services, which can hurt your cash flow and disrupt your practice.
Timely credentialing also helps you stay compliant with rules from both regulators and insurance companies, protecting you from fines or audits.
Most importantly, it builds patient trust. People feel more confident choosing a provider who is approved by their insurance and has verified qualifications. Keeping your credentials current helps you maintain a good reputation with patients, insurers, and regulatory bodies.
Concluding Words
Knowing the main types of medical credentialing, their provider, hospital, and payer credentialing helps healthcare professionals deliver quality care, follow the rules, and keep their practice financially healthy. Keeping credentialing accurate and up to date builds patient trust, protects your reputation, and ensures you get paid on time.
HMS Group Inc. offers easy, reliable credentialing services designed to fit your needs. We help you save time, avoid mistakes, and stay compliant. Contact us today to make your credentialing process smooth and stress-free.
FAQs
What are the main types of medical credentialing?
The main types are:
- Provider credentialing: Checking a doctor or healthcare provider’s qualifications.
- Hospital credentialing: Making sure providers meet hospital standards.
- Payer credentialing: Getting approved by insurance companies.
- Telehealth credentialing: Verifying online or remote healthcare providers.
- Vendor credentialing: Checking companies or suppliers that work with hospitals.
Why is provider credentialing important for doctors and physicians?
Credentialing for a doctor is important because it proves that a doctor is qualified, trained, and licensed to give safe medical care. Same credentialing for physicians goes. Without it, they can’t work in certain clinics, hospitals, or with insurance companies.
How does credentialing affect medical billing and reimbursements?
If a provider isn’t credentialed, insurance companies can reject or delay payments. Credentialing makes sure the provider is officially recognized, which helps billing go smoothly and payments come on time.
What is vendor credentialing for hospitals?
This is when hospitals check outside companies like medical supply vendors or service contractors, to make sure they meet safety, security, and quality standards before working in the hospital.
How often should medical credentialing be renewed?
Usually, credentialing needs to be renewed every 2–3 years. The exact time depends on state rules, insurance company policies, and healthcare facility requirements.