Insurance Credentialing For Therapists
Credentialing as a therapist involves becoming an approved or in-network provider for insurance companies in the USA. Providers encounter challenges in managing billing and enrolling for reimbursements from insurance. Insurance credentialing for therapists aim to work with insurance companies and boost their revenue cycle. Here’s a brief outline of the credentialing process for therapists.
Find Insurance Panels
Get started by researching and finding the insurance firms and panels you want to join. Create a list of ones you think are most appropriate to your particular practice as well as the customers you serve.
Get licensed and Certified
To be eligible for insurance certification, you must be licensed as a counselor or therapist in the state you reside in. Make sure you have all the required certificates and licenses required by the regulatory board of your practice.
National Provider Identifier (NPI)
A national provider identifier (NPI) number holder makes it possible for a provider to apply through the National Plan and Provider Enumeration System (NPPES) website.
Get Malpractice Insurance
Numerous insurance companies require that therapists be insured against malpractice before certifying their services.
Complete Provider Application
Each insurance provider will provide a separate provider application form. Complete the application correctly and include all the required documents that may comprise your driver’s license or certifications, NPI number and information about malpractice insurance.
Apply for the Insurance
When you’ve filled out the application and collected all the required documents, you can submit it to your insurance provider to be reviewed. Certain insurance companies have portals where you can submit your application electronically.
Waiting Time
The insurance credentialing for therapists can take some time. It’s not unusual for it to take from several weeks to a few months. During this time, insurance companies will examine your application, check the authenticity of your application, as well as perform an investigation into your background.
Negotiate Contracts
If insurance credentialing for therapists applications approve, the credentialing company will provide you with an agreement. Examine the contract carefully and if required, you can negotiate the reimbursement rates and other contract details.
Get In-Network Status
After you’ve signed the contract that you’ve signed, you will be considered to be an in-network partner for the insurance company. This means that you can take on patients covered by the insurer and receive direct payments from the insurer for services you offer.
Maintain Conformity
After you have become an in-network service provider, follow the guidelines and rules established by the insurance company which includes the proper documentation and billing procedure.
The process to obtain insurance credentials is lengthy and intricate, with the requirements varying among insurance companies. Certain therapists might employ credentialing experts to assist.
Some therapists choose not to participate in insurance credentialing because of administrative expenses, lower costs for reimbursement, or for other reasons. Take into consideration the specific requirements and goals of your practice prior to deciding to join an in-network network.
Importance of Insurance Credentialing for Therapists
A Broader Client Base
A lot of patients depend on health insurance plans to pay for therapy. In becoming an in-network service provider with different insurance companies, insurance credentialing for therapists can gain access to a more extensive client base and draw in people who may not have the funds to attend therapy because of financial limitations.
Greater Revenue Opportunities
As in-network insurance credentialing for therapists, therapists can be paid directly by insurance companies which can provide an increased and stable income stream. This also means that they do not have to rely on private-pay clients.
Credibility and Trust
Accreditation by insurance companies can improve the credibility of a therapist’s profession. It indicates that the therapist has met the standards and qualifications of the insurer and can increase confidence in potential clients.
Marketing Benefit
Being an in-network provider can be a powerful marketing tool. Being recognized as a trusted provider on the insurance company’s website can draw clients who look for therapists who are accepted by their insurance.
Client Retention
Clients with insurance coverage having an in-network service can increase the retention of clients. Patients are more likely to stay in therapy with a provider that accepts their insurance as it lowers their out-of-pocket costs.
Stability and Consistency
Collaboration with insurance firms can give therapists a stable and consistent client load. Stability can be beneficial for the long-term planning of business as well as financial security.
Community Referrals
Certain health professionals, such as primary care physicians, will often refer insurance credentialing for therapists that are connected to the insurance plan of the patient. Being accredited can result in more referrals from healthcare professionals.
Access to Insurance Panels
Specific insurance credentialing for therapists panel may be selective when accepting new providers. Through credentialing, therapists have access to these panels, which can be advantageous for collaboration and networking opportunities.
Differential Clients
By accepting a variety of insurance plans, therapists can work with patients who have different backgrounds, demographics and financial circumstances. This diversification can enhance therapists’ experience and help them understand clients’ needs.
Professional Growth
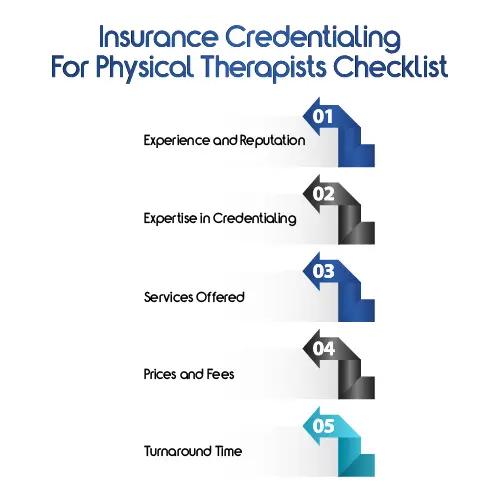
Insurance Credentialing For Physical Therapists Checklist
When seeking help from insurance credentialing for physical therapists, it is crucial to ensure that they provide complete and reliable assistance throughout the entire process of obtaining credentialing. Here’s a checklist of the critical aspects and services to take into consideration when evaluating the insurance credentialing for therapists:
Experience and Reputation
- Examine the company’s track record and expertise in therapist credentialing services.
- Check out testimonials from customers and reviews to assess their reputation and satisfaction with customers.
Expertise in Credentialing
- Make sure that insurance credentialing for physical therapists service has experience specifically in the process of certifying therapists.
- You must know the rules and regulations for different kinds of therapists (e.g. psychologists, counselors, social workers).
Services Offered
- Check the scope of services provided by HMS USA for the initial preparation of applications, enrollment of providers as well as re-credentialing and ongoing maintenance.
- Check if they help in Medicare or Medicaid enrollment and private insurance panels.
Prices and Fees
- Request a detailed list of all fees and expenses related to the process of obtaining credentials.
- Find out any additional costs for support, appeals, or changes on the application.
Turnaround Time
- Find out the average amount of time required for the insurance credentialing for physical therapists to complete the process.
- Ensure they have a reasonable timeframe for submitting applications and obtaining approval.
Common Mistakes to Avoid in Therapist Credentialing Services
Avoiding 5 common errors in the therapist credentialing services is essential to ensure efficient and successful credentialing. These are five common mistakes to look out for:
1. Incomplete or Incorrect Application Information
- Check that all sections of the enrollment form for providers are filled out accurately and completely.
- Double-check personal details such as licensing information, practice address and other contact details.
2. Not Supporting Documentation
- Examine the documentation requirements for the enrollment application carefully.
- Send all the necessary documents supporting your request, such as copies of certificates, licenses as well as malpractice insurance. National Provider Identifier (NPI) number if it is applicable.
3. Not Meeting Timelines
- The providers often have deadlines for application submission after the contract is granted.
- Inadvertently missing deadlines may delay enrollment which could hinder the ability of the provider to visit patients and get reimbursements on time.
4. Poor Follow-Up and Communication
- Keep track of the application status and contact the insurance company’s enrollment department if needed.
- A lack of communication can confuse as well as delays in the credentialing process.
5. Incorrectly verifying Insurance Panels
Before you begin the process of credentialing, make sure to check that the insurance panels are aligned with the goals of the therapist’s work.
Read More: Everything You Need to Know About Hospital Provider Credentialing Process.
Conclusion
Through partnering with professional services for credentialing therapists Practitioners can obtain professional advice on how to avoid mistakes that can be costly when it comes to credentialing. Examining insurance plans and negotiating favorable contract terms will help therapists make educated choices that are in line with their objectives for practice.
Insurance credentialing for therapists process offers the opportunity to grow in the field of counseling and mental health. A careful adherence to the process and avoidance of common errors allows counselors to be in-network providers and improve access to treatment for patients and encouraging an effective practice.