As the healthcare system becomes more complex, it’s more important than ever for doctors, hospital staff, and patients to understand the difference between hospital billing and physician billing. Billing is not easy at all because payer rules are always changing, regulations are always changing, and more people are using digital tools.
Understanding how hospital billing and physician billing function helps support accurate claim filing, proper reimbursement, and regulatory adherence. This blog will break down these two billing types and explain how each fits into the modern healthcare payment process.
What is Hospital Billing?
Hospital billing, also known as institutional billing, refers to the process through which healthcare institutions such as hospitals, outpatient clinics, rehabilitation centers, and skilled nursing facilities submit claims for the use of their facilities and services.
Institutional billing refers to charges for facility-related services rather than individual providers. It includes:
- Room and board
- Lab tests
- Radiology and imaging
- Operating and recovery room use
- Medical supplies and equipment
- Nursing services
- Pharmacy and ancillary services
These charges cover the infrastructure and resources used in patient care.
Hospital billing departments submit institutional claims typically to private insurers, Medicare, or Medicaid using the UB-04 (CMS-1450) form, designed to reflect the complexity of facility-based services.
What is Physician Billing?
Physician billing, also known as professional billing, refers to the process of submitting claims for services provided by individual healthcare providers—such as doctors, surgeons, and specialists.
It covers consultations, procedures, and other direct patient care and uses the CMS-1500 form for insurance reimbursement.
As healthcare becomes more specialized, understanding the distinction between hospital billing and physician billing is essential for providers, payers, and patients
Difference Between Hospital and Physician Billing
Hospital billing refers to charges for services provided by a healthcare facility, such as room and board, nursing care, lab tests, imaging, and equipment use. Most of the time, these are sent in on a UB-04 form.
On the other hand, physician billing is for professional services provided by particular providers, like consultations, procedures, or follow-ups. It is sent in on a CMS-1500 form. Hospital billing shows the cost of care received in a hospital, while physician billing shows the clinical work done by healthcare providers.
Understanding both is essential for accurate claim submission and reimbursement.
Definition of Professional Billing
Physician billing, often called professional billing, is the process by which private healthcare providers, such as doctors, nurse practitioners, and physician assistants, send in claims for the work they do.
This type of billing focuses on the professional components of care, typically rendered in outpatient settings such as private practices, clinics, or even within a hospital facility, but billed separately from institutional services.
What Physician Billing Includes
Physician billing includes services provided directly by licensed healthcare professionals, such as:
- Consultations and Evaluations: Office visits and follow-ups
- Procedures and Surgeries: Any surgical interventions by the physician
- Diagnostic and Therapeutic Services: Lab result interpretation, imaging, and treatments
- Ongoing Management: Chronic disease care and coordination
These services are coded using CPT and ICD-10 codes to indicate what was done and why.
Who Submits Physician Claims and To Whom
Physician claims are typically submitted by billing staff within a private practice or by a centralized billing office if part of a larger medical group. These claims are submitted to insurance payers, such as:
- Private health insurance companies
- Medicare
- Medicaid
- Workers’ compensation or other third-party payers
The accuracy of documentation and proper coding is essential for timely and appropriate reimbursement.
Associated Claim Form: CMS-1500
The CMS-1500 form is the standard document used to submit physician claims. This form, maintained by the Centers for Medicare and Medicaid Services, captures all relevant patient, provider, and service data required for processing the claim. Unlike the UB-04 form used in hospital billing, the CMS-1500 is tailored specifically for individual provider services.
Hospital Billing vs Physician Billing
Understanding the nuances between hospital and physician billing is essential for accurate claims submission and efficient reimbursement.
Below are the primary distinctions:
1. Type of Services Billed
Hospital Billing covers facility-related services such as inpatient stays, operating room use, laboratory tests, imaging, and nursing care.
Physician Billing includes services provided directly by healthcare professionals, such as consultations, office visits, and surgeries.
2. Billing Forms Used
Hospital Billing uses the UB-04 (CMS-1450) claim form.
Physician Billing uses the CMS-1500 claim form.
3. Billing Departments Involved
Hospital Billing is managed by the hospital’s centralized billing or revenue cycle department.
Physician Billing is typically handled by the individual provider’s office or medical group billing team.
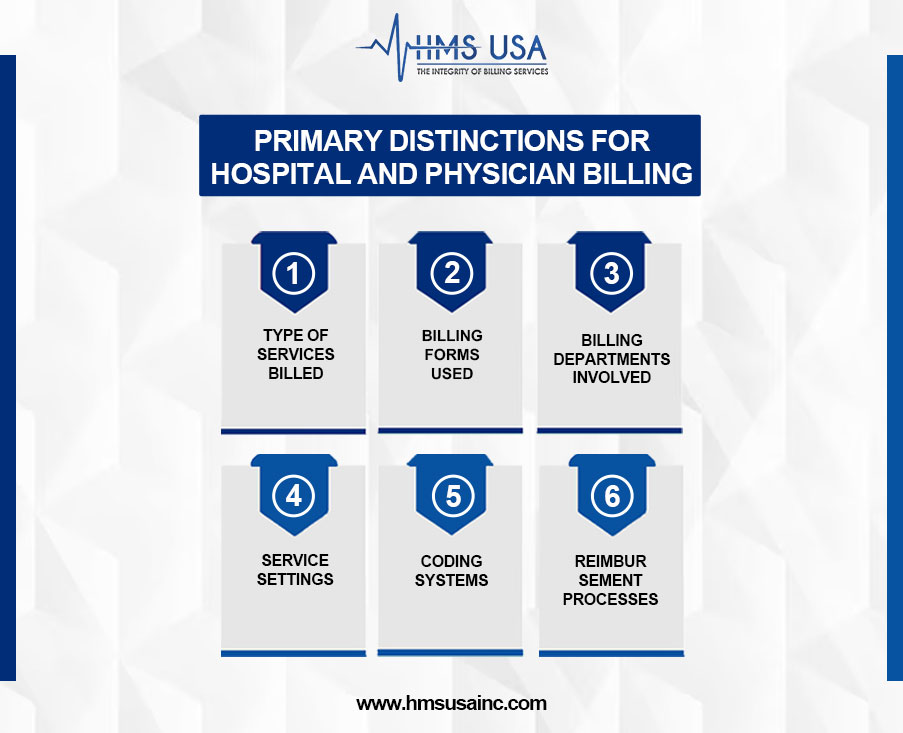
4. Service Settings
Hospital Billing applies to services rendered in inpatient, outpatient, and emergency room settings.
Physician Billing applies primarily to outpatient clinics, private practices, and hospital-based physician services (billed separately from the facility).
5. Coding Systems
Hospital Billing utilizes ICD-10, HCPCS, and Revenue Codes to define services.
Physician Billing uses CPT codes and ICD-10 codes to identify procedures and diagnoses.
6. Reimbursement Processes:
Hospital Billing often involves complex reimbursement models such as Diagnosis-Related Groups (DRGs) or bundled payments.
Physician Billing generally follows a fee-for-service or value-based reimbursement model, based on the services rendered.
Professional vs Institutional Claims
In medical billing, two primary claim types drive the reimbursement process:
- Professional claims
- Institutional claims.
Professional Claims (CMS-1500): Submitted by individual providers like physicians, nurse practitioners, and therapists for outpatient services such as consultations, evaluations, surgeries, and follow-ups.
Institutional Claims (UB-04): Submitted by facilities like hospitals, rehab centers, and nursing homes for services including room and board, lab tests, operating room use, and inpatient care.
When Is Each Claim Type Used?
Professional Claims are typically used when:
- A physician treats a patient in a private clinic or outpatient facility.
- A therapist offers individual therapy sessions.
- A specialist performs an outpatient procedure.
Institutional Claims are used when:
- A patient is admitted for inpatient care at a hospital.
- A hospital provides emergency room services.
- A skilled nursing facility offers long-term rehabilitation.
How Insurers Process Them Differently
Insurers handle professional and institutional claims differently due to their structure:
- Professional claims use CPT/HCPCS codes and are billed per individual service.
- Institutional claims use revenue codes, DRGs, and include facility fees, accommodation charges, and bundled payments.
Each claim type follows distinct review protocols and timelines, affecting approval and reimbursement speed.
Why the Difference Matters
For Providers and Coders
Correctly distinguishing claim types helps avoid billing errors, denials, and delays. Accurate coding ensures compliance and timely reimbursement.
For Patients
Patients may get separate bills from providers and facilities. Understanding this helps clarify multiple statements and EOBs.
To Prevent Billing Errors
Misclassified claims lead to rejections and revenue loss. Proper training and oversight support accurate billing and efficient revenue cycle management.
Concluding Words
Understanding the difference between professional and institutional claims is vital for accurate billing and timely reimbursement. Professional claims cover provider services, while institutional claims reflect facility-based care.
As billing complexities increase, proper claim classification helps avoid errors and improve financial outcomes. For expert support in optimizing your billing processes, contact HMS Group Inc. Our team specializes in both claim types and offers tailored solutions to enhance your revenue cycle.








