Claim denials continue to be a significant obstacle in medical billing, frequently delaying payments and placing financial pressure on healthcare providers. A denial occurs when a payer rejects a claim, either fully or partially, due to missing information, coding errors, or policy violations.
This is where denial reason codes come in. These codes provide clear explanations for why a claim was denied, giving billing teams the insights they need to fix issues, file appeals, and avoid repeat mistakes.
Why does this matter? According to a 2024 Change Healthcare report, 15% of medical claims are denied on the first submission, and shockingly, up to 65% are never resubmitted. That’s a huge revenue loss.
By understanding and acting on denial codes for medical billing, providers can improve claim success rates, speed up reimbursements, and protect their bottom line.
What Are Denial Reason Codes in Medical Billing?
Denial reason codes in medical billing are standardized alphanumeric or numeric codes assigned by insurance payers to communicate the reason for denying a medical claim. These codes are part of the adjudication process and help providers understand why reimbursement was withheld or reduced.
Each code includes a brief explanation of the denial reason, such as missing documentation, ineligible patients, duplicate services, or contractual issues, helping providers understand and resolve claim rejections effectively.
Categories/ List of Denial Codes
The arrangement of denial codes makes it easier to find and fix problems.
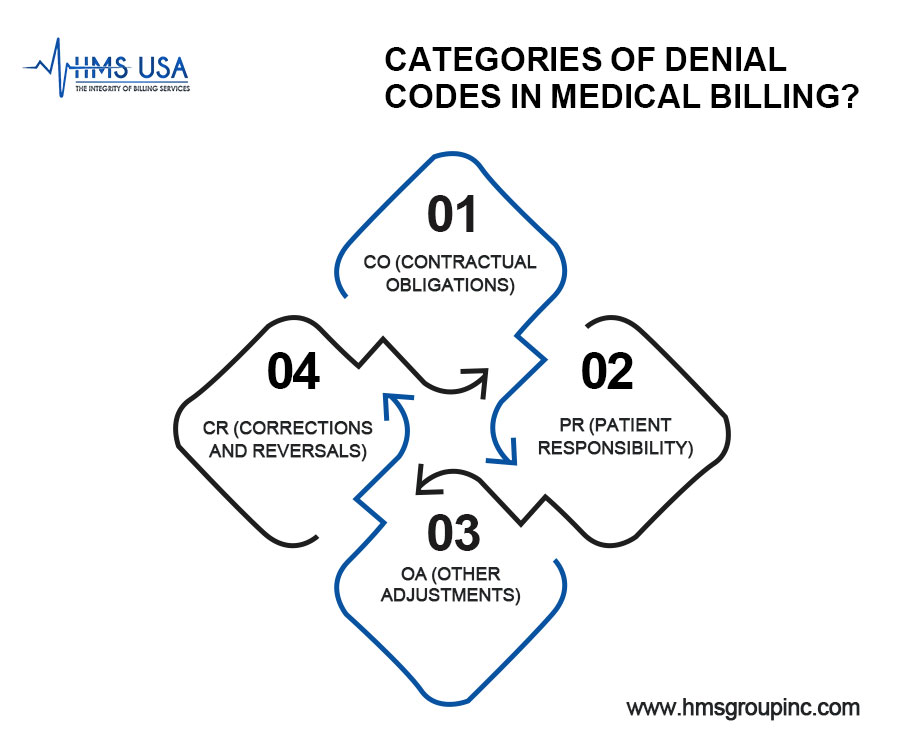
Common categories include:
- CO (Contractual Obligations): Amounts not payable due to prior agreements between payer and provider.
Example: CO 45 – Charge exceeds the fee schedule or contracted rate.
- PR (Patient Responsibility): The Amounts the patient owes, such as deductibles or copays.
Example: PR 1 – Deductible amount.
- OA (Other Adjustments): Adjustments not tied to patient responsibility or contracts.
Example: OA 18 – Duplicate claim/service.
- CR (Corrections and Reversals): Indicates a reversal or correction of a prior decision.
To understand and know how to respond correctly, it’s necessary to know about these categories.
Standardized Use by Payers
Most U.S. payers use standardized denial codes defined by CMS in the CARC and RARC lists. This standardization helps providers streamline denial resolution and use automation to fix common issues.
Understanding these denial codes enables providers to reduce administrative tasks, improve first-pass claim acceptance, and boost financial performance.
Top Common Denial Codes and Reasons in Medical Billing
Denial reason codes help medical providers identify why claims are rejected and how to fix them.
Two common codes are CO 22 and PR 227, each pointing to specific claim issues.
1. CO 22 – Coverage Not in Effect on the Date of Service
CO 22 Denial Code Description
The CO 22 denial code indicates that the patient did not have active insurance coverage on the date of service. This typically occurs due to eligibility issues, such as lapsed coverage, incorrect insurance details, or services rendered outside the policy’s effective period.
To resolve it, providers should verify insurance using real-time eligibility tools, correct any data entry errors, and resubmit the claim if active coverage is confirmed.
2. PR 227 Denial Code – Patient Did Not Provide Requested Information
This denial occurs when the insurer asks the patient for information (e.g., accident details, coordination of benefits, or student status) but receives no response. Providers should contact the patient, help them submit the required information, confirm with the insurer what is needed, and resubmit the claim once complete.
Additional Common Denial Codes and Reasons:
CO 16 – Claim/service lacks information which is needed for adjudication: Often related to missing modifiers, diagnosis codes, or clinical documentation.
CO 97 – The benefit for this service is included in the payment/allowance for another service/procedure: Indicates bundled services or unbundled billing practices.
CO 50 – These are non-covered services because this is not deemed a “medical necessity” by the payer: Usually requires submission of additional clinical justification or appeal.
Each of these denial codes serves as a communication tool between payers and providers, highlighting where corrective action is needed. Understanding these codes is vital for improving clean claim rates and reducing delays in reimbursement.
Root Causes of Denials
Addressing the root causes of claim denials is key to improving revenue cycle performance and minimizing administrative strain.
Common issues include:
- Inaccurate Patient Information
Errors in names, birth dates, or insurance details can trigger automatic denials.
Prevention: Train front-desk staff regularly and use patient verification tools before submission.
- Authorization or Eligibility Issues
Missing or incorrect pre-authorizations often lead to denials.
Prevention: Use a pre-authorization checklist and confirm requirements before providing services.
- Coding Errors or Modifier Mismatches
Incorrect CPT, ICD-10, or HCPCS codes or misuse of modifiers can result in denials.
Prevention: Employ certified coders, stay current with coding updates, and use coding audits.
- Late Claim Submissions
Claims filed past the payer’s deadline are usually denied with no appeal option.
Prevention: Track aging reports and automate filing deadline alerts.
Best Practices for Resolving Common Denial Medical Billing Issues
- Verification of Insurance and Pre-authorizations
Confirm patient eligibility and obtain required pre-authorizations before services are rendered to prevent eligibility-related denials.
- Staff Training and Coding Audits
Conduct regular training and audits to ensure accurate coding, proper documentation, and compliance with payer-specific guidelines.
- Using Billing Software and Denial Management Tools
Implement advanced billing software to detect errors, automate eligibility checks, and track denial trends for faster resolution.
- Timely Follow-up and Appeals Process
Establish a structured process for prompt follow-up and timely appeals to recover reimbursements and reduce claim backlogs.
Concluding Words!
Efficient denial management is about prevention as much as resolution. By understanding denial codes and implementing proactive measures such as accurate coding, thorough insurance verification, and staff training. Healthcare providers can increase claim approvals and protect their revenue.
To make lasting changes, work with medical billing experts. To lower denials, speed up collections, and simplify your revenue cycle so you can focus on giving great patient care, get in touch with HMS Group Inc.











