Medical billing is a crucial component of healthcare. It ensures that the care patients receive is properly linked to the payments healthcare providers rely on to operate. The process typically includes steps such as patient registration, VOB in Medical Billing, recording services, submitting claims, processing payments, and following up on outstanding amounts. Each step needs to be done correctly to avoid problems and delays.
One of the most important but sometimes overlooked steps is Verification of Benefits (VOB). This means checking a patient’s insurance before they get care to see what is covered and what the patient might have to pay.
VOB is not just a routine task; it helps make sure billing is accurate and payments come in on time. If this step is skipped or done wrong, it can lead to denied claims, delayed payments, and surprise bills for patients. That’s why VOB is such an important first step in the medical billing process.
What is VOB in Medical Billing?
VOB meaning in medical billing, is Verification of Benefits. It’s the process of checking a patient’s insurance details before they get medical care. This helps doctors and clinics know what the insurance will pay for and what the patient needs to pay out of pocket.
VOB is an important step in the billing process. When benefits are verified early, it helps avoid mistakes, reduces the chances of insurance claim rejections, and gives patients a clear idea of their costs.
During VOB, the provider checks important insurance details, such as:
Coverage: What services the insurance plan will pay for.
Copay: The set amount the patient pays for things like doctor visits or prescriptions.
Deductible: The amount the patient has to pay before the insurance starts covering costs.
Out-of-Pocket Limit: The most a patient will have to pay in a year; after that, the insurance pays everything.
The VOB Process in Medical Billing
Verification of Benefits (VOB) is one of the first and most important steps in the medical billing process. It helps healthcare providers understand what services a patient’s insurance will cover before any treatment begins. This ensures fewer billing surprises for both patients and providers.
Step-by-Step Guide to the VOB Process
1. Collecting Patient Information
The provider gathers basic personal and insurance details from the patient, usually when they book an appointment or check in.
2. Requesting Insurance Verification
The office staff or billing team contacts the insurance company to check the patient’s benefits. This can be done by phone, through online portals, or using special billing software.
3. Reviewing the Insurance Response
The insurance company sends back information about what is covered. The team reviews this carefully to confirm the patient is eligible for services.
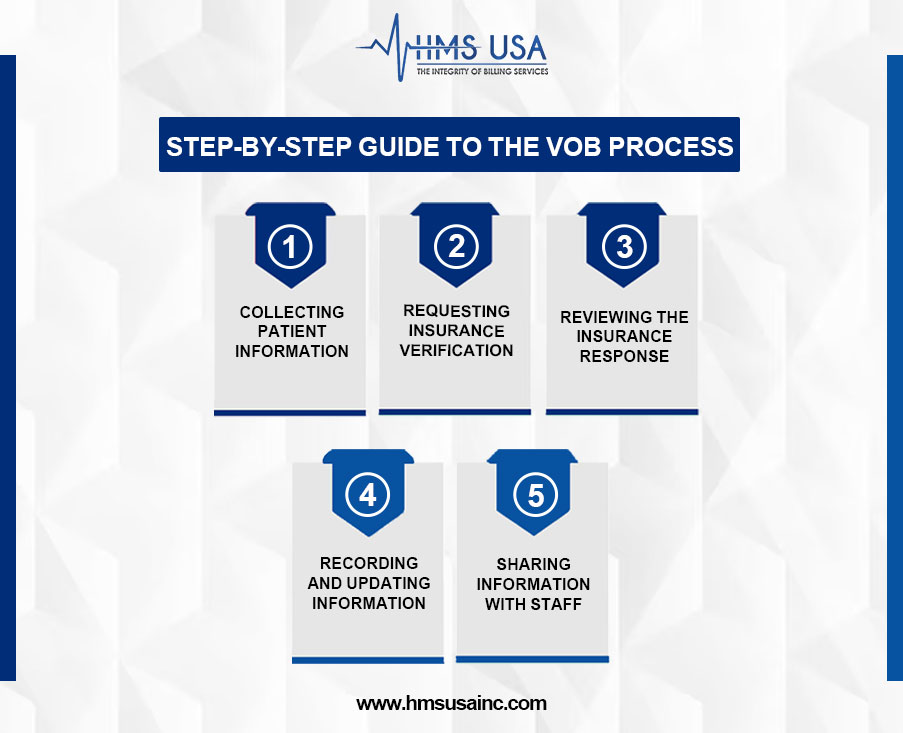
4. Recording and Updating Information
All insurance details are saved in the patient’s file. If there are any unclear or missing details, the team follows up with the insurer or the patient.
5. Sharing Information with Staff
The verified insurance details are shared with doctors and billing staff. This helps with treatment planning and lets patients know what to expect in terms of costs.
What Information Is Verified During VOB?
- If the insurance policy is active
- What services are covered, and any limits
- Copay and coinsurance amounts
- How much of the deductible has been met
- If pre-approval (authorization) is needed
- Any services that are not covered
- The out-of-pocket maximum for the year
Why Communication with Insurance Is Important?
Good communication with insurance companies is key to avoiding billing errors. Staff may call the insurer or use online systems to get real-time updates on any changes to the patient’s coverage or requirements for treatment approval.
Why Verification of Benefits (VOB) Matters in Medical Billing
Verification of Benefits, or VOB, is an important step in medical billing. It’s not just paperwork; it helps make sure healthcare providers get paid properly and patients understand what their insurance covers.
Helps with Accurate Billing
VOB confirms if the patient’s insurance will cover the services before they are given. Without this step, the provider might send a bill that gets denied because of wrong or missing information. Doing VOB right from the start helps avoid mistakes and billing problems later.
VOB Catches Issues Early
VOB helps find issues like:
- Insurance that has ended or is no longer active
- Changes in the insurance company or plan
- Services that need approval before being done
- Whether the provider is in the insurance network or not
By spotting these early, providers can take the right steps, like getting approvals or letting the patient know about possible costs.
Prevents Billing Issues and Delays
If VOB isn’t done correctly, it can lead to:
- Denied claims
- Delays in payment
Tools and Technologies Supporting Smooth VOB Operations
Healthcare providers use several helpful tools to make the Verification of Benefits (VOB) process easier and more accurate.
These include electronic systems that check insurance eligibility (like EDI 270/271), practice management software, and clearinghouses that collect and organize insurance information. Many offices also use automated VOB tools to reduce mistakes and save time. These technologies help providers work more efficiently, avoid billing errors, and stay in line with insurance rules.
Key Benefits of Accurate and Timely VOB
Verification of Benefits (VOB) means checking a patient’s insurance details before they receive care. Doing this on time and correctly helps both the healthcare provider and the patient. Here’s how:
- Confirms Insurance Coverage Early
Checking insurance before the visit helps avoid surprises, like claim rejections or unpaid bills.
- Improves Cash Flow and Reduces Denials
When coverage is confirmed upfront, there are fewer billing issues, and payments come in faster.
- Builds Patient Trust
Patients feel more confident when they know what their insurance will cover and what they’ll need to pay.
- Helps with Treatment Planning and Approvals
Understanding what the insurance covers helps plan the right care and get any needed pre-approvals in advance.
Best Practices for Effective VOB
A strong VOB process helps avoid mistakes and delays. Here are some simple steps to follow:
- Collect Complete Patient Information Early
Get all the patient’s insurance and personal details when the appointment is scheduled.
- Verify Insurance with Portals or Phone Calls
Use online insurance tools or call the insurance company to confirm coverage, limits, and copayments.
- Keep Records and Update Changes Quickly
Write down all verification details and update them right away if anything changes.
- Train Your Staff Well
Make sure your team knows how to check insurance correctly and stays up to date on insurance rules
Common Challenges in VOB and How to Overcome Them
Inconsistent Payer Information: Insurance details may be outdated or conflicting, requiring repeated follow-ups.
Long Wait Times & System Limits: Delays in reaching payers or using outdated tools can slow billing and scheduling.
How to Overcome these Challenges
- Use tools integrated with EHR or billing systems to speed up verification.
- Assign trained staff to focus solely on VOB tasks.
- Outsource to experienced billing partners for improved accuracy and reduced workload.
Wrap-up!
Verification of Benefits (VOB) is an important step that helps healthcare providers check a patient’s insurance coverage before giving care. When done correctly and on time, VOB helps doctors plan better, keeps patients informed about their costs, and makes billing run more smoothly.
Working with experts like HMS Group Inc. can make your VOB process easier and more reliable. We help reduce claim denials, improve communication with patients, and support the financial health of your practice. Let us help you make VOB simple and effective.
FAQs
What does VOB mean in medical billing?
VOB stands for Verification of Benefits, a process where a provider confirms a patient’s insurance coverage details before delivering services.
Why is the VOB process in medical billing important?
The VOB process helps avoid claim denials, ensures the provider gets paid correctly, and informs patients about their financial responsibility upfront.
What information is gathered during a VOB?
VOB includes verifying policy status, deductible amounts, copay details, coverage limits, exclusions, and any pre-authorization requirements.
How does VOB catch issues before treatment?
By verifying insurance in advance, VOB catches issues like expired policies, non-covered services, or unmet deductibles, reducing billing errors.
What are the best practices for smooth VOB operations?
Use automated tools, verify early, document thoroughly, and train staff regularly to ensure smooth VOB operations and accurate billing.









