Facing more claim denials than ever? You’re not alone. As healthcare regulations tighten in 2025, providers are up against tougher payer requirements and stricter documentation rules.
To stay ahead, healthcare organizations must adopt smart, proactive denial management strategies that not only recover revenue but also protect the flow of patient care and keep the revenue cycle strong.
This blog explores the fundamentals of denial management in healthcare, common denial causes, the importance of understanding denial reason codes in medical billing, and offers practical tips and best practices to enhance your approach this year.
Understanding Denial Management in Healthcare
Denial management in healthcare refers to the systematic process of identifying, analyzing, and resolving medical claim denials issued by insurance companies. It is a critical component of revenue cycle management (RCM), as denied claims can delay payments, reduce cash flow, and increase administrative burden.
A proactive denial management strategy begins with understanding the root causes of denials. These commonly include:
- Incomplete or incorrect patient information
- Missing or invalid prior authorizations
- Non-covered services under the patient’s insurance
- Coding errors, including incorrect ICD-10 or CPT codes
- Late claim submissions
Successful denial management needs to look at the denial reason codes. The data collected from the payer explains why claims are being turned down. Reviewing and categorising them regularly helps find trends so that you can take steps to stop future denials.
2025 Technology Trends in Denial Management
In today’s dynamic healthcare environment, denial management is essential, not optional. With constantly changing payer policies and value-based reimbursement models, timely denial prevention is critical to a practice’s financial health.
By 2025, providers are adopting advanced technologies and integrated systems to minimize denials and improve revenue cycle performance. Key trends include:
1. AI and Automation in Denial Management
AI and automation streamline tasks like claim status checks, denial categorization, and follow-ups. These tools help identify denial patterns, reduce manual workload, and address root causes more effectively.
2. Real-Time Eligibility Verification
Verifying insurance coverage and benefits before service delivery prevents denials due to eligibility issues. Integrating these tools into front-end workflows ensures cleaner claims and faster processing.
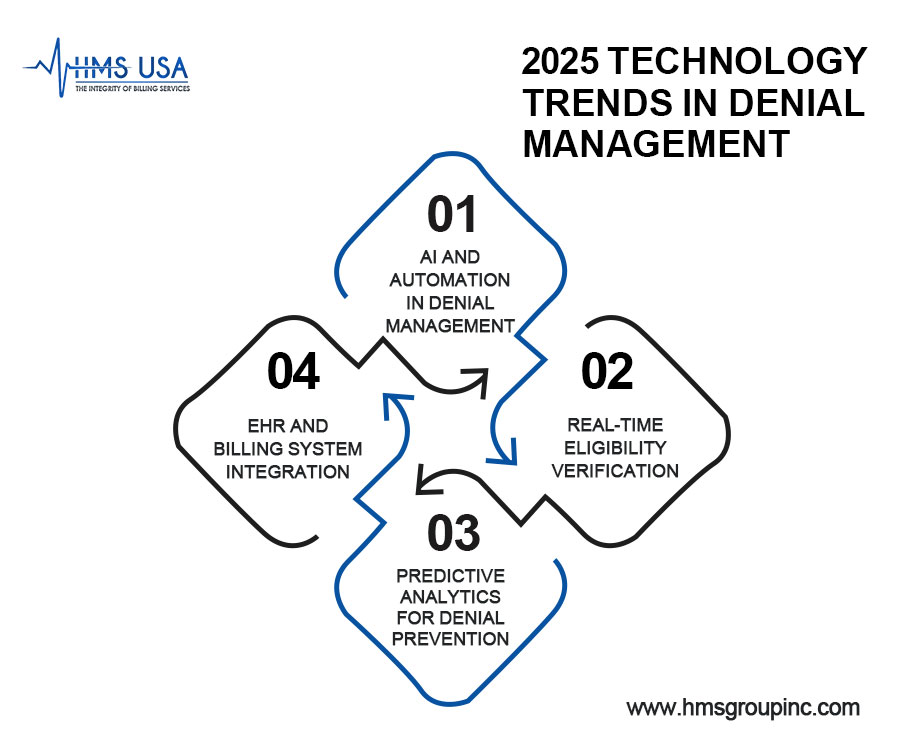
3. Predictive Analytics for Denial Prevention
By analyzing historical and real-time data, predictive analytics identifies high-risk claims and flags potential issues before submission, allowing proactive corrections and improving claim success rates.
4. EHR and Billing System Integration
Linking EHRs with billing systems eliminates data silos, improves accuracy, and streamlines workflows. This integration minimizes documentation errors and reduces denials due to mismatched or incomplete data.
Proven Denial Management Strategies for Reducing Claim Denials
Modern technology is important, but basic recommended practices are still important for managing denial effectively. The following tried-and-true methods can assist in lowering the number of claim denials and enhancing payment outcomes:
1. Strengthen Front-End Processes
Accurate patient data, insurance verification, and pre-authorization checks at the front end minimize eligibility-related denials and ensure smoother claim processing.
2. Ensure Coding Compliance and Documentation Accuracy
Keep coding teams updated with ICD-10, CPT, and HCPCS guidelines. Accurate documentation supports compliant coding, increasing claim approval rates.
3. Train Staff on Denial Reason Codes
Regular training on interpreting denial reason codes helps billing teams resolve issues quickly and avoid repeat denials. Understanding payer-specific rules is key to timely corrective action.
4. Use Real-Time Claim Editing Tools
Claim editing software flags errors like missing modifiers or invalid codes that are before submission, allowing staff to correct issues and prevent denials.
5. Standardize Appeals and Follow-Up
Consistent appeal templates, tracking systems, and automated reminders help meet deadlines, improve denial overturn rates, and reveal underlying process issues.
Key Metrics to Monitor for an Effective Denial Management Strategy
Tracking key performance indicators (KPIs) is vital for identifying denial trends and improving revenue cycle outcomes:
- Denial Rate
Measures the percentage of claims denied. A high rate signals issues in billing, coding, or data entry.
- First-Pass Resolution Rate
Indicates how many claims are paid without rework. High rates reflect strong front-end processes like accurate coding and verification.
- Days in Accounts Receivable (A/R)
Tracks the average time to receive payment. Fewer days mean efficient billing; delays may suggest denial or follow-up issues.
- Appeal Success Rate
Shows how often denied claims are successfully appealed. Low rates may indicate weak documentation or slow response times.
- Root Cause of Denials
Identifying denial causes, such as coding errors or authorization issues, helps target workflow improvements and staff training.
Call us today or visit www.hmsgroupinc.com to schedule a consultation. Let us help you turn denials into opportunities for improvement and growth.
Best Practices for a Successful Denial Management Plan
Go beyond reactive resubmissions with these proactive healthcare denials management strategies:
- Cross-Functional Collaboration
Unite billing, coding, and clinical teams to ensure claim accuracy and reduce denials.
- Monthly Denial Audits
Review and analyze denials regularly to detect patterns and apply corrective actions.
- Denial Tracking by Payer
Monitor denials by insurance providers to tailor processes and staff training to specific payer rules.
- Proactive Insurer Communication
Maintain clear, timely communication with payers to resolve issues and prevent repeat denials.
- Stay Updated on Payer Policies
Continuously monitor changes in insurance guidelines to ensure compliance and reduce policy-related denials.
Key Mistakes to Avoid in Claim Denial Management
- Failing to analyze historical denial data leads to repeated mistakes and missed improvement opportunities.
- Undertrained staff struggle with coding and payer rules, increasing the risk of denials.
- Submitting appeals late often results in missed deadlines and lost revenue recovery.
- Relying on manual processes limits efficiency and weakens denial tracking and resolution efforts.
Final Words
As denial management in healthcare reimbursement changes, it’s more important than ever to know how to handle denials well. Organisations can reduce denials and improve their financial results by using data, following proven procedures, and avoiding common mistakes.
Success now hinges on investing in skilled personnel, optimized workflows, and advanced technology. A proactive, tech-enabled approach not only minimizes claim rejections but also enhances the patient experience with faster, more accurate reimbursements. Continuous improvement and adaptability will be key to staying ahead in 2025 and beyond.
To stay competitive in today’s healthcare environment, providers must prioritize proactive, data-driven denial management strategies. Investing in the right processes, technology, and team collaboration can significantly reduce denials, improve cash flow, and strengthen your overall revenue cycle.
Looking to optimize your denial management process?
Contact HMS Group Inc. for expert solutions tailored to your organization’s needs. Our experienced team can help you implement efficient workflows, leverage analytics, and improve your denial resolution rates.