Claim denials happen when an insurance company refuses to pay a medical bill, either in part or in whole. In OB/GYN practices, this can slow payments, create extra work for staff, and confuse patients.
Handling denials carefully helps the practice stay financially healthy, run smoothly, and keep patients satisfied. In this read, we are going to discuss the common reasons for medical claim denials in healthcare and strategies to prevent them.
Common Reasons for Claim Denials in OB/GYN Billing
Claim denials create administrative burden and cash-flow risk for OB/GYN practices. The most frequent causes of denials in OB/GYN billing include coding errors, missing patient or insurance data, lack of prior authorization, duplicate claims, and insufficient clinical documentation. Below are the typical failure points and how they translate into denials:
1. Coding Errors
Incorrect CPT/HCPCS selection, wrong modifiers, or outdated procedure codes (for example, C-section coding errors) are a top driver of denials. Train coders on OB/GYN-specific edits (bundling rules, global maternity periods) and run pre-bill scrubs targeted to high-risk codes.
2. Missing or Incorrect Patient Information
Simple entry errors, wrong DOB, policy ID, or payer name, lead to immediate rejections. Verify insurance at check-in and again at pre-op scheduling; automate demographic validation via the EMR where possible.
3. Missing Prior Authorizations
High-cost procedures, advanced imaging, and elective surgeries often require payer pre-approval. Build an authorization tracker with reminders tied to surgery dates.
4. Duplicate Claims or Billing Mistakes
Duplicate charges for the same encounter or improper bundling of services often show up as payer edits. Use clearinghouse duplicate checks and reconcile daily charge batches.
5. Not Enough Documentation
When notes do not support medical necessity (e.g., reason for cesarean), payers deny. Standardize operative notes and use documentation templates linking diagnosis codes to CPTs.
Best Strategies to Reduce Claim Denials
Reducing denials in OB/GYN billing requires a combination of front-end accuracy, technology, and continuous process improvement. Implement these key strategies:
1. Front-End Verification & Authorization
Verify eligibility, benefits, and prior authorization requirements at scheduling and again at check-in. KPI: 98% eligibility verified before service.
2. Accurate Coding + Specialty Checklists
Create OB/GYN coding checklists for common procedures (prenatal visits, delivery types, postpartum care). Require a coder sign-off for all high-risk codes (C-section CPTs). KPI: Reduce coding denials by 30% in 90 days.
3. Pre-Bill Claim Scrubbing
Use claim-scrubbing software tuned to OB/GYN payer edits (global maternity edits, NCCI pairs). Integrate scrubs into the EHR to catch issues before batch transmission.
4. Documentation Templates and Clinical Nudges
Adopt EHR templates that prompt clinicians to capture required elements: gestational age, indication for C-section, counseling notes, and informed consent. This directly reduces medical-necessity denials.
5. Denial Triage and Analytics
Create a denial dashboard that categorizes denials by code/reason and payer. Assign owners and SLAs (e.g., respond to high-value denials within 48 hours). KPI: days-to-resubmission <14 days.
6. Ongoing Staff Training
Quarterly training on OB/GYN coding updates, payer policy changes, and modifier use (e.g., 22, 59, 25, where clinically appropriate).
7. Regular Audits and Peer Review
Conduct monthly claim audits focused on high-risk areas (C-sections, global surgical periods, bundled maternal care) to catch systemic issues early.
8. Communicate with Payers
Maintain open communication with insurance companies to clarify ambiguous rules, resolve coding discrepancies, and confirm claim requirements. Early communication can prevent denials and speed up payment processing.
9. Audit Claims Regularly
Conduct periodic internal audits of submitted claims to ensure compliance with payer rules and regulations. Audits help detect errors early, improve documentation practices, and strengthen your denial prevention strategy.
OB/GYN practices can prevent claim denials and keep payments on track by using correct codes, checking patients’ insurance coverage, using helpful technology, and training their staff regularly. This also helps patients have a smoother experience.
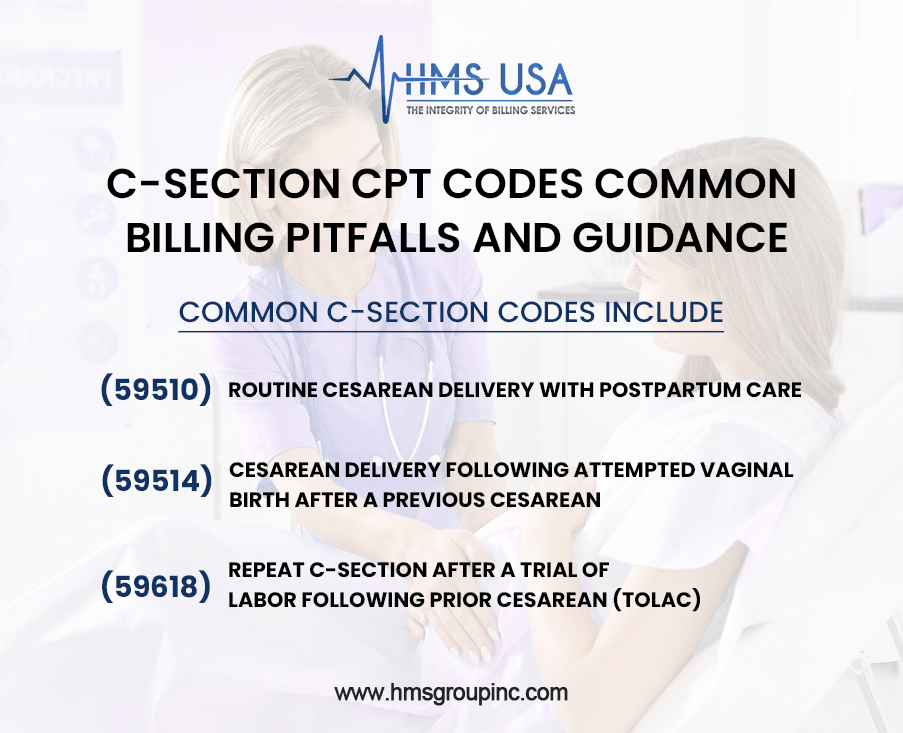
C-Section CPT Codes — Common Billing Pitfalls and Guidance
Correctly billing cesarean deliveries avoids frequent denials and payment delays. Common C-section CPT codes and tips:
Common C-section codes include:
- 59510 — Routine cesarean delivery with postpartum care. Use when cesarean is primary and the postpartum global period applies.
- 59514 — Cesarean delivery following attempted vaginal birth after a previous cesarean. Document VBAC trial and indication.
- 59618 — Repeat C-section after a trial of labor following prior cesarean (TOLAC). Use with appropriate modifiers if required.
Pitfalls to avoid:
- Billing a global maternity code incorrectly alongside separate anesthesia or facility charges.
- Forgetting to add modifiers for distinct procedures performed the same day (document clinical rationale).
- Not linking the obstetric diagnosis (e.g., placenta previa, fetal distress) to justify surgical delivery often triggers medical necessity denials.
Recommendation: Maintain a short OB/GYN CPT cheat sheet in the coding workflow and require concurrent clinical documentation review for all cesarean claims.
If denials are hurting your cash flow, contact HMS Group Inc. for specialized OB/GYN medical billing and denial prevention services.
How Technology Helps Reduce OB/GYN Claim Denials
Modern tech is a force multiplier for OB/GYN billing teams. Obgyn medical billing benefits from EMR integrations, eligibility APIs, and automated claim scrubbing. Key technologies:
- Eligibility & benefits verification APIs (real-time checks at scheduling)
- Pre-bill scrubbing engines customized to maternity edits and DRG/bundling rules
- Denial analytics dashboards that show top denial reasons (e.g., coding vs prior auth) and dollars at risk
- Workflow automation to route authorizations, append clinical notes, and trigger appeals
Outcome: fewer preventable denials, shorter days-in-AR, and more predictable revenue.
Specialized Considerations in OB/GYN Billing
OB/GYN billing has unique complexities:
Global maternity bundles: surgeries and postpartum care are often bundled; ensure timing and service splits are correct.
High-risk deliveries: NICU follow-ups and neonatal services may require separate claims — coordinate between maternal and infant billing teams.
Telehealth and prenatal remote monitoring: confirm payer rules for telehealth maternity visits and remote fetal monitoring codes.
Modifier use: Use modifiers for distinct services (modifier 59, 25, 22) only when documentation supports separation.
Document these policies in an OB/GYN billing manual and review them during monthly revenue meetings.
Key Metrics to Track for Denial Prevention
To measure progress against denials in OB/GYN billing, track:
- Denial rate (denials / total claims) by payer and by procedure (target <5–7% depending on payer mix)
- Denial-to-recovery ratio ($ recovered / $ denied) — shows appeal effectiveness
- First-pass acceptance rate — aim for >90% with strong scrubs
- Days in AR — target <45 days for OP, <60 days overall
- Top 10 denial codes and dollars lost — monitor monthly and assign owners
Use these KPIs to drive improvement cycles and calculate ROI for technology/investments.
Bottom Line
Managing denials in OB/GYN billing demands a proactive front-end, specialty-aware coding, effective technology, and continuous staff education. When your team combines eligibility checks, OB/GYN-specific coding controls (for C-sections and maternity bundles), and a focused denial management workflow, denials drop, and cash flow stabilizes.
If your practice needs operational support, HMS Group Inc. offers specialized OB/GYN medical billing and denial management services to reduce denials and improve revenue performance.
FAQs
What are the top reasons for denials in OB/GYN billing?
Coding mistakes, incorrect patient or insurance info, missing prior authorizations, duplicate claims, and insufficient documentation are the most common causes.
Which CPT codes are commonly used for C-section billing?
Common C-section CPT codes include 59510, 59514, and 59618—each has distinct documentation and global period implications.
How can we reduce medical necessity denials for C-sections?
Include clear operative indications (e.g., fetal distress), relevant imaging/lab results, and documented counseling; use templates to ensure consistency.
How fast should denials be reworked?
Aim to triage high-value denials within 48 hours and resubmit corrected claims within 14 days.
When should an OB/GYN practice consider outsourcing billing?
Consider outsourcing when the denial rate >10%, days-in-AR remain high (>60 days), or internal staff lack payer-specific expertise.











