Claim edits in medical billing act as automated checkpoints that verify claims before submission. They identify errors like missing data, incorrect CPT or ICD-10 codes, and incomplete patient details, issues that often lead to claim denials. By fixing these problems upfront, claim edits improve claim accuracy and ensure faster reimbursements.
In a fast-moving healthcare system, timely payments matter more than ever. Claim edits support your revenue cycle management (RCM) by ensuring clean claim submission. This not only protects your financial stability but also allows healthcare providers to stay focused on patient care, not billing rework.
As a trusted medical billing company in the USA, HMS USA INC uses smart edits and compliance-driven workflows to help practices achieve higher claim acceptance rates and stronger cash flow.
What Are Claim Edits in Medical Billing?
Claim edits are automated rules built into your billing software to validate claims before submission to payers. These rules check for coding accuracy, coverage criteria, and compliance with payer policies.
Think of them as a digital safety net that prevents costly denials. For example, if a CPT code doesn’t match the diagnosis or if documentation is missing, claim edits will flag the issue immediately, before the claim reaches the insurer.
Clean claims mean faster payments, fewer rejections, and better financial performance for healthcare providers.
Why Claim Edits Matter
Protecting Revenue and Reducing Denials
Every denied claim represents delayed revenue and extra administrative work. That’s why claim edits play such a vital role; they detect potential denial triggers before submission.
When claims are accurate and compliant, providers experience faster reimbursement cycles and improved cash flow. This efficiency allows billing teams to focus on proactive denial prevention rather than reactive rework.
Strengthening Compliance and Accuracy
Claim edits also ensure alignment with payer-specific requirements, Medicare guidelines, and National Correct Coding Initiative (NCCI) edits. This helps your organization maintain compliance, avoid audits, and uphold accuracy in billing documentation.
Understanding Medicare NCCI Edits
The Medicare National Correct Coding Initiative (NCCI) edits, developed by CMS, are crucial in maintaining proper coding standards. These edits prevent incorrect code pairings and ensure services are billed appropriately.
For instance, certain CPT code combinations can’t be billed together unless specific conditions are met. NCCI edits flags such issues automatically, protecting your practice from denials and compliance risks.
Following Medicare NCCI edits not only keeps your billing compliant but also reinforces trust with payers, ensuring claims are processed quickly and correctly.
Types of Claim Edits in Medical Billing
Claim edits fall into several categories, each addressing different aspects of claim accuracy and compliance.
1. Coding Edits (CPT/ICD-10)
These check whether diagnosis and procedure codes align logically. Mismatched codes often trigger immediate rejections, so these edits ensure proper code pairing.
2. Duplicate Edits
They identify duplicate billing for the same patient, provider, or service date, preventing accidental overbilling and audit risks.
3. Bundling/Unbundling Edits
Certain services must be billed together under one comprehensive code. Bundling edits catches cases where separate codes are used incorrectly.
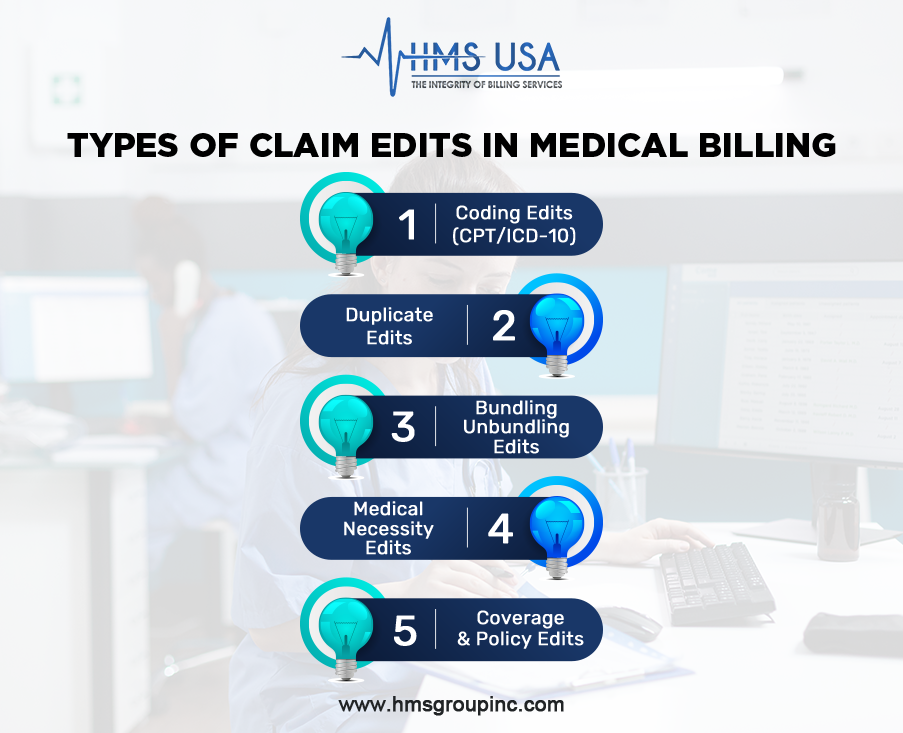
4. Medical Necessity Edits
These ensure services are supported by the patient’s diagnosis and medical necessity documentation. Unsupported claims are flagged for review.
5. Coverage and Policy Edits
They confirm that the patient’s insurance plan covers the service. Frequency limits and coverage restrictions are checked to avoid rejections.
By implementing these types of claim edits in medical billing, practices can greatly reduce denials and improve first-pass acceptance rates.
Claim Edits in RCM – Revenue Cycle Management
Claim edits play a critical role in the success of your revenue cycle management (RCM) strategy.
Before Claim Submission
Smart edits catch errors in real time, ensuring every claim is “clean” before being sent to payers. This step alone can reduce denials by up to 40%.
After Denials Occur
When denials happen, claim edits help identify patterns, revealing if certain codes, providers, or payers are frequently causing issues.
Integrated with Technology
Modern billing systems use AI-driven smart edits to automate error detection. These tools enhance billing accuracy while saving time and labor costs.
Collaboration and Workflow
Successful RCM depends on teamwork. Billers, coders, and clinicians must communicate clearly to ensure that all clinical details match the coding and documentation.
By using claim edits effectively, HMS USA INC helps healthcare providers reduce denials, strengthen cash flow, and achieve financial efficiency.
How Claim Edits Differ from Claim Audits
It’s common to confuse claim edits with claim audits, but their purposes differ:
| Item | Claim Edits | Claim Audits |
| When It Happens | Before claim submission | After submission or payment |
| How It Works | Automated software validation | Manual or detailed post-review |
| Goal | Prevent denials and ensure accuracy | Verify compliance and identify billing trends |
| Benefit | Faster payment and fewer rejections | Long-term accuracy and accountability |
Both are essential, but claim edits act as your first line of defense, ensuring clean claims and timely reimbursement.
How Smart Edits Prevent Denials and Protect Revenue
Smart edits combine automation and intelligence to eliminate billing errors before they impact your bottom line.
Benefits include:
- Fewer Denials: Catching issues early prevents resubmissions and revenue loss.
- Faster Payments: Clean claims get approved quickly by payers.
- Stable Cash Flow: Predictable revenue supports better business planning.
- Higher Staff Productivity: Teams spend less time correcting claims and more time managing growth.
By implementing smart claim edit systems, HMS USA INC ensures clients experience reduced AR days and higher claim approval rates, turning billing into a streamlined revenue engine.
Best Practices for Reducing Claim Errors
1. Regular Staff Training
Billing guidelines, CPT codes, and payer policies evolve frequently. Continuous training keeps your billing team up-to-date and compliant.
2. Internal Claim Audits
Conducting routine audits helps identify recurring claim issues and improve process accuracy.
3. Use Smart Billing Software
Investing in technology with automated claim edits ensures accuracy from the start. Smart software minimizes manual review and speeds up billing cycles.
4. Partner with Experts
Outsourcing your billing to a trusted medical billing company like HMS USA INC ensures compliance, accuracy, and timely reimbursements through expert handling.
Conclusion
Claim edits in medical billing are more than just a technical step—they are a financial safeguard. By catching errors before submission, they protect your revenue, reduce denials, and accelerate cash flow.
To maintain accuracy and compliance:
- Keep staff trained and informed
- Use billing software with smart edits
- Partner with professionals who understand payer-specific requirements
If your practice struggles with denials or cash flow gaps, HMS USA Inc. can help. As one of the most trusted medical billing services in the USA, we specialize in:
- Claim management and denial prevention
- RCM optimization
- Provider credentialing services
- Affordable medical billing services for all specialties
Contact HMS USA INC today to optimize your claims process, improve accuracy, and protect your practice’s financial health.
FAQs
What are claim edits in medical billing?
Claim edits are automated checks that identify errors or missing information before claim submission, ensuring accuracy and preventing denials.
How do claim edits prevent denials?
They detect incorrect coding, missing documentation, or non-covered services before submission, allowing corrections that improve first-pass rates.
What are Medicare NCCI edits?
These are CMS coding rules that prevent improper billing combinations, ensuring correct code usage and compliance with federal guidelines.
What are the main types of claim edits?
Coding edits, duplicate edits, bundling/unbundling edits, medical necessity edits, and coverage edits are the most common.
How can HMS USA Inc. help my practice?
HMS USA INC provides denial management services, claim scrubbing, and smart RCM solutions to reduce errors, improve reimbursements, and enhance financial performance.