The ICD-10 coding system (International Classification of Diseases, 10th Revision) serves as the global standard for documenting and identifying medical conditions. Within mental health care, it ensures consistent diagnosis, proper treatment planning, and accurate billing.
ICD-10 Code F33.1 represents Major Depressive Disorder (MDD), recurrent, moderate. This means an individual has experienced multiple episodes of moderate depression impacting their emotional stability and daily activities. Correct documentation of this diagnosis is crucial for ensuring quality care, transparent medical records, and successful insurance claims processing.
Understanding ICD-10 Code F33.1 – Recurrent Depressive Disorder, Moderate Episode
ICD-10 Code F33.1 identifies recurrent moderate depression. It applies to individuals who have experienced previous depressive episodes and are currently facing moderate symptoms that interfere with productivity, motivation, and social life, but without delusions or hallucinations.
In simpler terms, this code highlights the return of depression symptoms that disrupt day-to-day functioning without reaching severe or psychotic intensity.
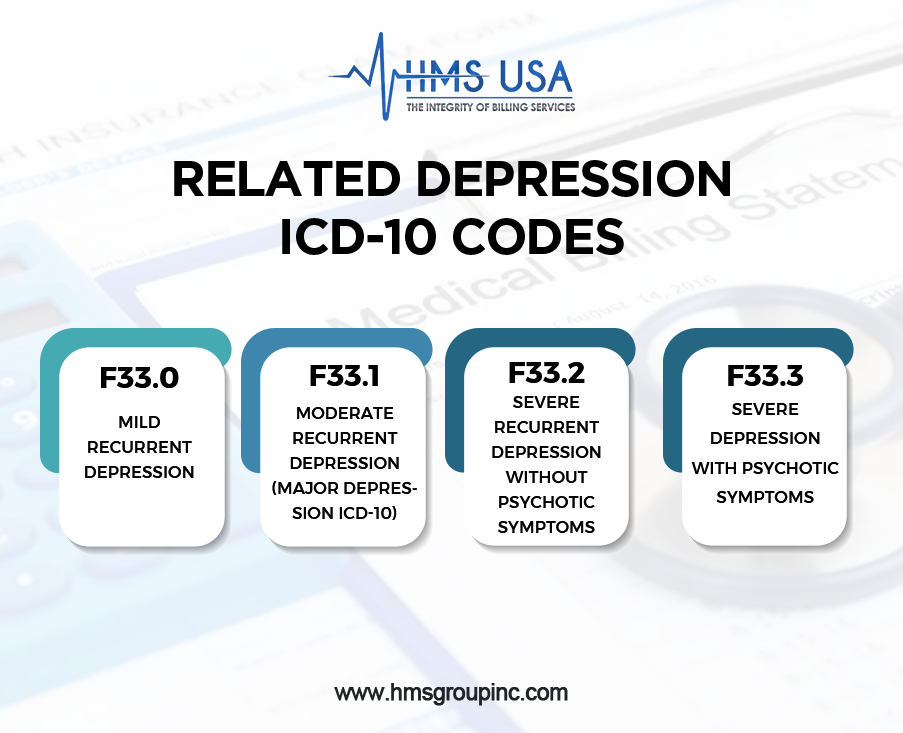
Related Depression ICD-10 Codes
- F33.0: Mild recurrent depression
- F33.1: Moderate recurrent depression (major depression ICD-10)
- F33.2: Severe recurrent depression without psychotic symptoms
- F33.3: Severe depression with psychotic symptoms
Choosing the correct code, like F33.1, ensures accurate documentation, targeted treatment, and smooth insurance reimbursement.
Major Depressive Disorder (MDD) – What It Means
According to the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders), Major Depressive Disorder is characterized by persistent sadness, loss of interest, and significant functional impairment.
To meet the diagnostic criteria, symptoms must last for at least two weeks and mark a noticeable change from an individual’s usual behavior.
Common symptoms of moderate recurrent depression (F33.1):
- Persistent sadness or irritability
- Loss of interest in daily activities
- Fatigue or low energy
- Difficulty concentrating or making decisions
- Changes in sleep or appetite
- Feelings of guilt or worthlessness
While not as intense as psychotic depression, F33.1 still impacts daily life, work, and relationships. Proper coding and treatment planning help ensure that individuals receive appropriate therapeutic or pharmacological interventions and insurance coverage.
DSM-5 Criteria for Major Depressive Disorder
The DSM-5 criteria outline that a diagnosis of Major Depressive Disorder requires five or more symptoms lasting at least two weeks, with one being either a depressed mood or loss of interest in pleasurable activities.
Typical symptoms include:
- Persistent sadness or emptiness
- Fatigue or low energy
- Sleep or appetite changes
- Feelings of guilt or hopelessness
- Impaired focus
- Thoughts of death or suicide
In the ICD-10 system, depression is categorized by severity:
- F33.0 – Mild
- F33.1 – Moderate
- F33.2 – Severe (without psychotic symptoms)
Healthcare providers often use standardized scales like the PHQ-9 and Hamilton Depression Rating Scale (HDRS) to measure severity and ensure accurate alignment with both DSM-5 and ICD-10 standards.
Documentation and Coding Guidelines
Accurate use of ICD-10 Code F33.1 begins with clear, evidence-based clinical documentation. Providers must include:
- Symptom descriptions and duration
- Impact on daily functioning
- Recurrence or previous episodes
Common coding errors include:
- Using F32.x codes (single episodes) instead of F33.x (recurrent episodes)
- Omitting severity level (mild, moderate, or severe)
- Incomplete documentation of episode history
Good documentation practices improve claim approval rates and clinical outcomes. Providers should describe symptom onset, progress, treatment outcomes, and any recurrence patterns.
Common Clinical Scenarios Using ICD-10 Code F33.1
F33.1 applies to patients with more than one depressive episode, where current symptoms moderately affect daily life.
Example:
A patient treated for depression two years ago now presents with fatigue, sadness, and decreased motivation lasting several weeks, without psychosis. The correct code: F33.1 (Major Depressive Disorder, Recurrent, Moderate).
Depression coding summary:
- F32.x → single depressive episode
- F33.x → recurrent depression
- F33.0 → mild
- F33.1 → moderate
- F33.2 / F33.3 → severe
Proper classification ensures effective treatment and smooth insurance processing.
Treatment and Management Approaches
Treating recurrent moderate depression (F33.1) requires a multidisciplinary, evidence-based approach.
Common Treatments
Most patients benefit from combination therapy, a mix of medication and psychotherapy.
- Medication: SSRIs and SNRIs regulate serotonin and norepinephrine levels.
- Therapy: Cognitive Behavioral Therapy (CBT) and Interpersonal Therapy (IPT) help restructure thought patterns and improve coping skills.
- Advanced treatments: In resistant cases, ECT (Electroconvulsive Therapy) or TMS (Transcranial Magnetic Stimulation) may be used.
Role of Medication, Therapy, and Lifestyle
- Medication: Helps balance mood and energy.
- Therapy: Encourages self-awareness and emotional management.
- Lifestyle: Regular exercise, a healthy diet, and sufficient sleep support long-term recovery.
Pro Tip: Integrating mindfulness, social connections, and structured routines greatly enhances treatment outcomes.
Importance of Follow-Up Care
Follow-up appointments allow providers to track progress, adjust treatment, and prevent relapse. Coordinated care among psychiatrists, therapists, and primary care physicians ensures a supportive network for patient recovery.
For expert support with ICD-10 coding, mental health documentation, and insurance reimbursement, contact HMS USA Inc., your trusted partner for compliant, precise, and efficient mental health billing services. Get a Free Consultation Today!
ICD-10 Code F33.1 in Billing and Reimbursement
Why Accurate Coding Matters
Accurate coding directly impacts insurance reimbursement and claim approval. Using the correct code, F33.1, ensures the diagnosis aligns with the provided treatment, preventing denials and delays.
How Coding Works with EHR Systems
Modern Electronic Health Record (EHR) systems integrate ICD-10 codes to minimize human error, streamline billing, and maintain documentation accuracy.
Meeting Insurance Requirements
Insurance payers require documentation consistency. Providers should ensure that all progress notes, treatment plans, and evaluations align with the diagnosis code F33.1. Regular coding audits prevent compliance issues and claim rejections.
Key Differences Between ICD-10 and DSM-5 Classifications
The ICD-10 and DSM-5 serve distinct yet complementary purposes:
- ICD-10 (by WHO) classifies health conditions globally for medical and billing purposes.
- DSM-5 (by APA) defines mental health conditions through diagnostic criteria.
In short:
- DSM-5 identifies what the condition is.
- ICD-10 provides the code to document and bill for it.
Using both ensures clinical accuracy, clear communication, and efficient healthcare delivery.
Conclusion
ICD-10 Code F33.1 is vital for identifying and managing Major Depressive Disorder (Recurrent, Moderate). Accurate documentation supports better patient outcomes, ensures compliance, and simplifies reimbursement.
Staying updated with DSM-5 and ICD-10 standards minimizes coding errors and strengthens clinical workflows.
FAQs
What does ICD-10 Code F33.1 represent?
It stands for Major Depressive Disorder, Recurrent, Moderate, episodes of depression that moderately affect daily functioning.
How is F33.1 different from other depression-related ICD-10 codes?
F33.1 indicates recurrent moderate depression, while codes like F32.0 or F33.2 describe different severity levels.
What are the DSM-5 criteria for MDD?
Five or more symptoms (e.g., low mood, fatigue, poor concentration) for two weeks or more, including depressed mood or loss of interest.
Why is accurate coding important?
It ensures compliance, correct billing, and continuity of care.
Can F33.1 be used for insurance billing?
Yes, when properly documented, it supports accurate reimbursement and claim processing.











