Credentialing is a critical process that ensures healthcare providers are fully qualified, licensed, and verified to deliver safe patient care. It serves as the foundation for legal compliance and smooth reimbursement.
In this detailed guide, we’ll break down the cost of credentialing for a healthcare providers, explain how it works, and highlight ways to reduce expenses through expert help from HMS USA INC.
What Is Credentialing in Healthcare?
Credentialing, meaning in healthcare,e is the process of verifying a provider’s qualifications, including education, licenses, certifications, and professional history. It ensures that every healthcare professional, from physicians to therapists, meets the standards required by insurance payers and regulatory bodies.
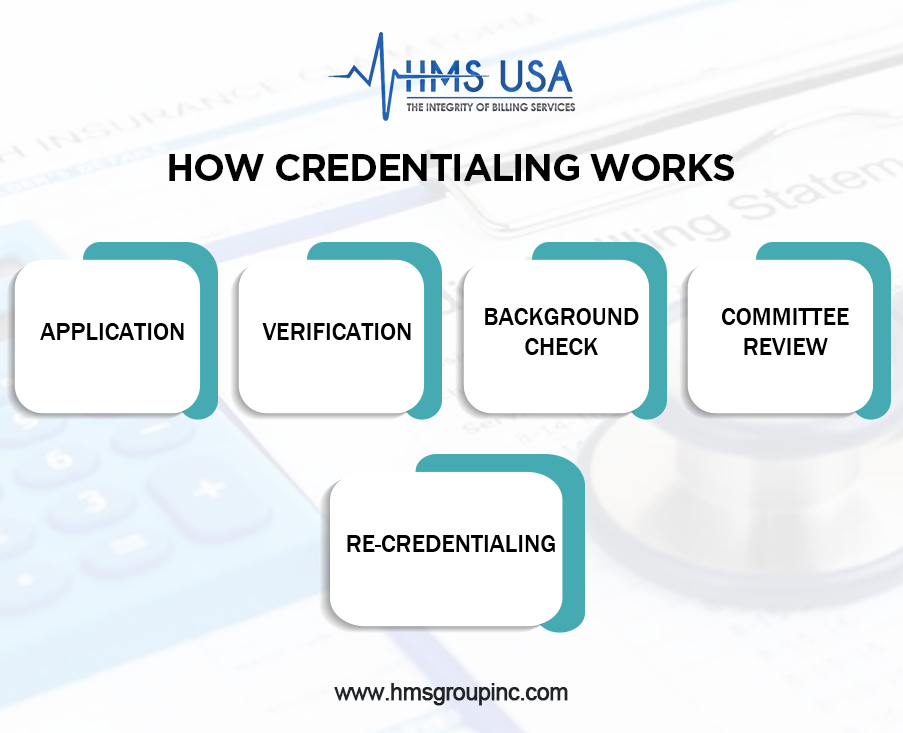
How Credentialing Works
- Application: The provider submits education, certification, and work history.
- Verification: A credentialing specialist confirms details with schools, licensing boards, and governing authorities.
- Background Check: Malpractice history and disciplinary records are reviewed via databases like NPDB.
- Committee Review: Experts review the verified data and approve participation.
- Re-Credentialing: Every 2–3 years, providers must renew to maintain compliance.
Credentialing vs. Enrollment vs. Privileging
| Process | Purpose | Outcome |
| Credentialing | Verifies provider qualifications | Confirms eligibility for clinical practice |
| Enrollment | Registers providers with payers | Enables billing and reimbursements |
| Privileging | Authorizes specific procedures | Defines the scope of care |
Each step is crucial to ensure safe care, steady reimbursements, and operational compliance.
Why Credentialing Matters
Credentialing protects patients, boosts facility credibility, and ensures providers can legally bill insurers. It also reduces audit risk and compliance penalties.
In short:
- Builds trust between patients and providers.
- Protects healthcare organizations from legal risks.
- Ensures timely payment from insurance companies.
- Promotes a culture of transparency and safety.
Ready to stay compliant and get paid faster? Get a free credentialing audit with HMS USA Inc. today.
The Role of a Credentialing Specialist
A credentialing specialist plays a vital role in managing all documentation, verifications, and renewals. They ensure accuracy, meet deadlines, and maintain compliance.
Key Responsibilities:
- Collect provider credentials and licenses.
- Complete payer-specific applications.
- Submit and track insurance enrollments.
- Handle re-credentialing and renewal reminders.
By outsourcing to an experienced specialist, you minimize delays, reduce administrative workload, and prevent costly denials.
Understanding the Cost of Credentialing for Healthcare Providers
The cost of provider credentialing services varies based on multiple factors:
| Factor | Impact on Cost |
| Provider Type | Solo practitioners usually pay less than large groups. |
| Number of Networks | More insurance panels = higher cost and complexity. |
| State Regulations | Some states require additional verifications and background checks. |
| Process Type | Manual workflows cost less upfront but create errors and delays. |
| Labor Time | The longer it takes, the higher the cost. |
Typical pricing:
- Per payer: $200–$1,000
- Full-service packages: $1,500–$3,000
- Re-credentialing: $150–$400 (depending on documentation)
In-House vs. Outsourced Credentialing
| Option | Pros | Cons |
| In-House Credentialing | Full control, direct communication with payers. | Requires trained staff, software, and more time. |
| Outsourced Credentialing | Experts handle everything, faster results, fewer errors. | Service fee, but higher ROI due to faster reimbursements. |
Outsourcing is often the smarter investment, especially for growing practices and multi-provider organizations.
Don’t let credentialing slow your cash flow; let HMS USA Inc. handle your medical credentialing from start to finish.
Why Credentialing Services Matter
Medical credentialing services ensure compliance with all payer and regulatory standards. They manage every step, from CAQH registration to re-credentialing, ensuring you stay active and bill without interruptions.
Benefits include:
- Faster approvals from payers.
- Fewer claim denials and rejections.
- 100% compliance with licensing rules.
- Smooth re-credentialing reminders and updates.
How to Estimate Your Credentialing Costs
Before budgeting, consider:
- How many providers or locations need enrollment?
- Is it for initial credentialing, re-credentialing, or both?
- How many insurance networks will you join?
- Will you use provider credentialing services or manage in-house?
For a single provider, expect an average of $150–$300 per payer, plus verification fees and potential software costs.
Common Mistakes That Increase Credentialing Costs
Avoid these frequent errors that delay approvals:
- Submitting incomplete or incorrect applications.
- Missing renewal or re-credentialing deadlines.
- Failing to update provider information in CAQH.
- Lack of follow-up with insurance networks.
Pro Tip: Automate reminders and track renewals using credentialing management tools or professional services.
How Credentialing Specialists Save Time and Money
Credentialing specialists streamline applications, prevent compliance lapses, and manage timelines effectively. Their expertise in payer rules helps avoid rejections, saving both time and revenue.
Want to know how much time your practice can save with expert help? Schedule a free consultation with HMS USA Inc. now.
How Often Do You Need to Re-Credential?
Most insurance companies require re-credentialing every 2–3 years. Costs depend on the number of payers and whether you handle it internally or outsource. Required documents typically include:
- Updated licenses and certifications
- Recent malpractice history
- Active NPI and DEA information
- Updated CV and references
Timely re-credentialing ensures uninterrupted billing and keeps your provider status active.
Tips to Manage Credentialing Costs Effectively
- Automate tasks: Use RPA or credentialing software to track expirations.
- Centralize data: Keep provider credentials and payer details organized.
- Outsource smartly: Delegate to experts for accuracy and efficiency.
- Stay proactive: Monitor payer policies regularly to prevent compliance issues.
Final Words
Credentialing is more than an administrative task; it’s a compliance necessity that drives your revenue cycle. Knowing the cost of credentialing for a healthcare providers, planning renewals, and leveraging medical credentialing services helps ensure you stay compliant and profitable.
Whether you’re a solo practitioner or manage a large group, HMS USA INC simplifies provider enrollment, reduces errors, and accelerates payer approvals.
FAQs
What is credentialing in healthcare?
Credentialing is the process of verifying a provider’s education, license, and qualifications to ensure they meet payer and regulatory standards.
How much does credentialing cost for healthcare providers?
The cost of credentialing for healthcare providers typically ranges from $200–$1,000 per payer, while full-service credentialing can cost $1,500–$3,000.
What does a credentialing specialist do?
A credentialing specialist handles applications, verifies documents, and ensures providers stay compliant with payer requirements.
How often is re-credentialing required?
Providers are usually re-credentialed every 2–3 years to maintain active status with insurance networks.
Is outsourcing credentialing worth it?
Yes. Outsourcing to medical credentialing services saves time, reduces errors, and ensures faster payer approvals.