In recognition of Mental
Health Awareness Month
Get a Free Healthcare
Billing Audit Now
Only for Mental Health Service Providers!
lets discuss your
Medical Billing Audit Deficiencies



Mental Health Awareness
Month Offer
Limited Time Offer: Free Audit services untill may 31st
Mastering Behavioural Billing Audit For
Mental Health Professionals
- HMS USA ensures legal compliance and accuracy in Behavioural billing audits, promptly identifying and rectifying any concerns to prevent harm.
- Different sorts of audits can be done, prospective before the claim is submitted, retrospective after the claim is billed, and concurrent during the billing process.
- HMS USA’s billing audits are designed to eradicate, rectify, and detect errors, ensuring accurate claims processing and full compliance with payer and state regulations.
- Reviews often focus on code documentation, which could lead to payer non-coverage or overpayment.
- The review audit process checks Behavioural records, claims, and billing papers for compliance with doctor’s reports, codification standards, and payer regulations.
Mental Health Billing Issues
Mental health billing can be complicated. Due to complex insurance requirements that vary by provider, mental health providers often struggle. Coding problems often delay or deny claims. These issues can hurt a practice’s revenue and viability.

Stop Massively Overpaying on Behavioural Claims
Get a Free Healthcare Billing Audit Now
How can we Help!
How Can we Help!

Challenges Faced by Professionals in Mental Health Billing

Patient Benefit Plan Issues
Mental health providers often struggle with patient benefit plans, leading to payment delays. HMS tackles this by investigating, verifying, and negotiating insurance coverage, ensuring smoother reimbursements and fewer delays.

Coding errors like Correct DX/CPT
DX and CPT code selection might be difficult for professionals. One erroneous code can delay payments, deny claims, and even audits! But fear not—HMS will save the day. We keep up with coding concerns to ensure your codes are accurate.

Claims Rejections And Denial
Mental health practitioners often face insurance claim denials. Our specialists complete claims, handle pre-authorizations, and resolve denials quickly by eliminating payment delays and administrative burdens.

Complex Insurance Regulations
Insurance regulations for mental health care vary by insurance company and can be complicated. HMS simplifies complex insurance regulations for mental health care, ensuring accurate documentation and compliance, thus minimizing audit risks.

Requirements Of Documentation
Insurance companies require thorough mental health service paperwork. HMS prevents claim denials and audits with extensive documentation.

Payment Scheduling
In the realm of Behavioral health billing, providers contend with the complexities of payment and fee schedules, striving to strike a balance between financial stability, patient affordability, and regulatory compliance.
Take Control of Your Billing Today!
Register for a Behavioural billing audit of your practice before May 31 to discover how your billing can be more profitable and administrative functions automated. Mental Health Awareness Month inspired us to launch this deal.
Through this limited time offer, you won’t lose this unique opportunity to evaluate your current practice’s RCM, discovering strengths, and weaknesses, as well as areas for improvement and potential cost savings.
Our experts will team up with you to build a custom plan that will target collections and billing in order to achieve the goal of maximizing your reimbursement.
Don’t miss out on this opportunity to take control of your billing and improve the financial health of your practice. This Offer is Valid for Mental Health Practices only!
Sign up for your free audit today!
What Our Clients Say About Us!

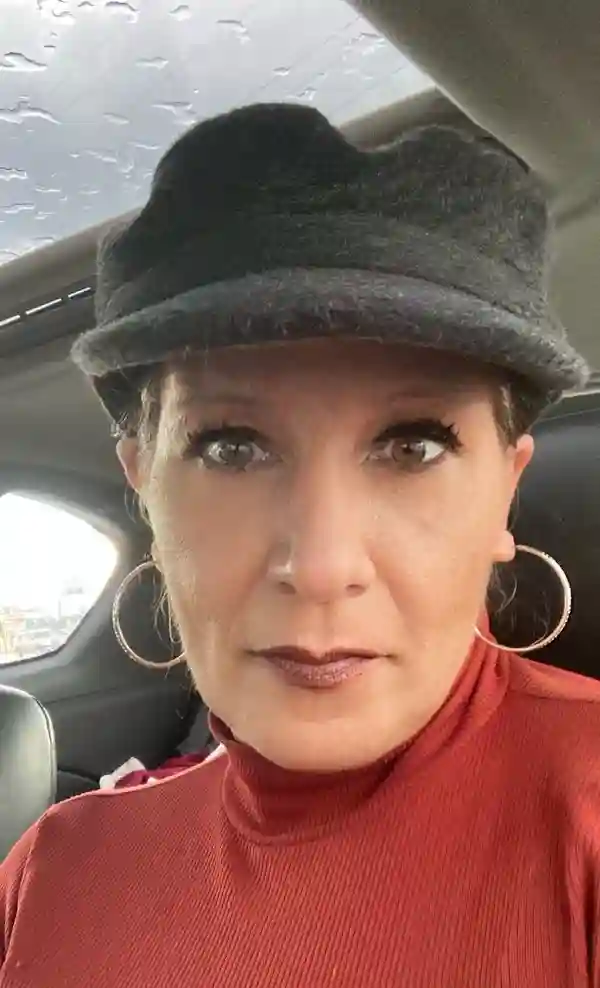
Cheryl Gray
Getting Better Counseling Services“HMS has gone beyond our imagination, when it comes it optimizing our billing. Their medical billing specialists have deep know how of billing regulations and standards taht help us navigate the maze of billing.Additionally we were able to get the customer support whenever we needed, which greatly amplified our practice operations. We highly recommend HMS, if you want someone to streamline your billings and ensure timely payments.”
Alesha Shaheen-Wiliams
Michigan Psychoanalytic Services"We are amazed by the medical billing services from HMS. With their assistance, we were able to increase our revenue and reduce costs. HMS professional team was always available to help us overcome all the hurdles all the way. With their superior knowledge and expertise, we were able to streamline our billings, which helped us put our practice on path to success. So, without any doubt, HMS is our go to medical billing company."
FAQS
Complex insurance restrictions, coding problems, claim denials, and patient benefit plan concerns plague mental health professionals. These issues might reduce revenue and increase administrative work.
A Behavioural billing audit can assist mental health practitioners fix coding problems, streamline claim submission, and comply with insurance rules. It can simplify billing and boost income.
Behavioural billing audits are vital to mental health providers’ finances. They can increase revenue by fixing problems. Audits reduce claim denials, ensure insurance compliance, and boost billing efficiency.
Mental health provider patient benefit plan challenges are HMS USA’s specialty. Their focused strategy reduces reimbursement delays, allowing providers to focus on patient care.
HMS USA monitors coding issues to ensure appropriate DX and CPT code selection, preventing payment delays, claim denials, and audits.


